Before modern pharmacy an early treatment for Rheumatoid Arthritis (RA) was cod liver oil, rich in omega-3 fats and vitamin D. A 2013 study demonstrated that consumption of cod liver oil resulted in a reduction of daily diclofenac in Rheumatoid Arthritis. As early as 1959 cod liver oil was recommended for arthritis in the medical literature. A 2017 review of marine omega-3 fats for arthritis pain found moderate quality evidence in rheumatoid arthritis patients. A 2024 review of prevention and treatment for RA suggested that a diet rich in fiber, vitamins, omega 3 and low glycemic index foods contributes to protection from RA. A comprehensive review of omega-3 fatty acids for RA included analysis of several studies and concluded that omega-3 was a valuable therapeutic option to improve pain symptoms, tender joint count, duration of morning stiffness and the frequency of NSAID consumption. A 2019 review of cumulative data on omega-3 fats to combat autoimmune diseases concluded:
“The promising findings coming from the cumulative research work over the last decade solidified the role of ω-3 PUFAs as a potential candidate to prevent or even treat such autoimmune diseases as type 1 diabetes, RA, SLE, MS”
A 2024 review of marine omega-3 PUFA (polyunsaturated fatty acids) for RA reported:
“Altogether the data reported in this review show that anti-inflammatory interventions, i.e., high fish consumption or supplements containing n-3 PUFAs, should be the standard of care, along with pharmacotherapy, in treating patients with RA.”
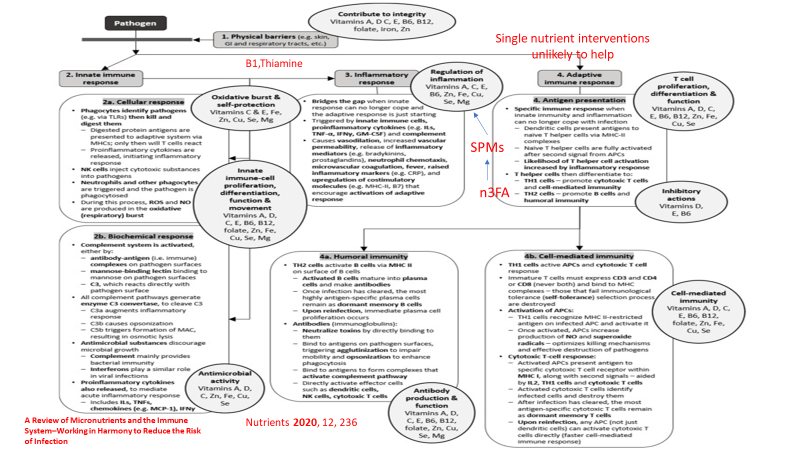
And here is a graphic from that article showing the effect of SPMs (specialized pro-resolving mediators, derived from omega-3s):

What about osteoarthritis?
A multicenter randomized double blind placebo controlled trial of krill oil containing 0.60 g EPA/d, 0.28 g DHA/d, 0.45 g astaxanthin/d demonstrated improvements in pain, stiffness and physical function.
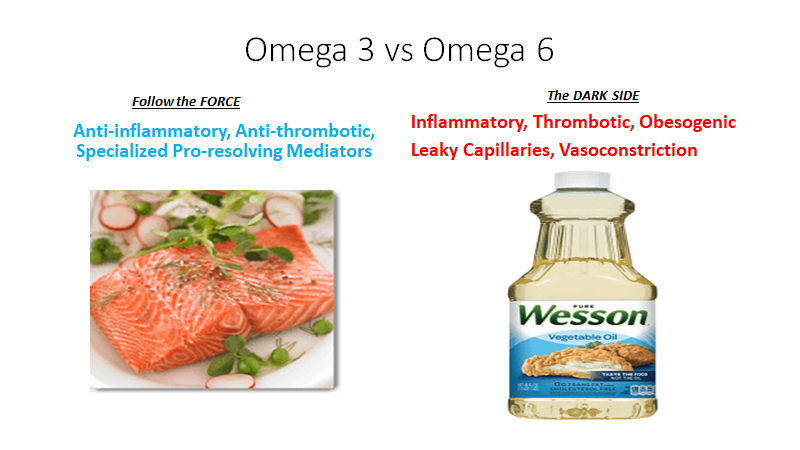
Some omega-3 supplement studies have demonstrated no significant pain relief in osteoarthritis. Those studies did not reduce the consumption of pro-inflammatory n-6 fatty acids which compete with omega-3 fats for the enzymes which can lead to pro or anti-inflammatory mediators. They also did not measure the omega 6/omega 3 ratio in blood or tissues. Nor did they measure the omega-3 index (% of omega-3 achieved in red blood cell membranes, the gold standard for evaluating tissue levels achieved) This 2018 analysis stated:
“High Omega-3 (n-3) polyunsaturated fatty acids (PUFAs) are associated with lower levels of inflammatory mediators, anti-nociception, and adaptive cognitive/emotional functioning. High Omega-6 (n-6) PUFAs are associated with inflammation, nociception, and psychological distress. While findings related to n-3 supplementation in knee OA are mixed, consideration of the n-6:n-3 ratio and additional outcome measures may provide improved understanding of the potential relevance of these fatty acids in OA”
The authors went on to access blood n-6/n-3 ratios in patients with OA and found the following:
“The high ratio group reported greater pain and functional limitations, (all p’s<0.04), mechanical temporal summation (hand and knee, p<0.05), and perceived stress (p=0.008) but not depressive symptoms.”
“In adults with knee pain, a high n-6:n-3 ratio is associated with greater clinical pain/functional limitations, experimental pain sensitivity, and psychosocial distress compared to a low ratio group.”
The anti-inflammatory diet that I follow and recommend eliminates the major sources of excess omega-6 in the diet, specifically the “vegetable oils” which are actually seed, grain, and legume oils predominated by soy oil, corn oil, peanut and cottonseed oil present in cooking “vegetable oils” and processed foods. A table that displays the ratio of omega 3 to omega 6 in various oils can be found here. Note that this table does not reveal the amounts of MUFA (mono unsaturated fatty acids) which are arguably “heart healthy”. Nor does it address the important issue of protective polyphenols and anti-oxidants (such as in Extra Virgin Olive oil aka EVOO). So do not make choices of oil based only on the omega-3/6 ratio.
Another consideration in choosing oils for cooking (as opposed to salad dressing) is the smoke point. Under high heat, oils are subject to oxidation which creates a proinflammatory effect when consumed. Refined Avocado oil has the highest smoke point (520 degrees F). But we digress. Back to pain and arthritis.
An article just published in Nutrients reviewed Omega-3 Supplementation and Its Effects on Osteoarthritis.
“omega-3 polyunsaturated fatty acids (PUFA) have demonstrated an influential role in the progression of OA, resulting in the reduction of cartilage destruction, inhibition of pro-inflammatory cytokine cascades, and production of oxylipins that promote anti-inflammatory pathways.”
“Research has demonstrated a positive effect on the modulation of OA symptoms through diet and exercise to promote an anti-inflammatory environment. More specifically, omega-3 PUFAs have demonstrated a reduction in inflammatory biomarkers and cartilage degradation, counteracting the natural disease state of OA. In addition to their chondroprotective role, omega-3 supplementation has been shown to have indirect positive effects on muscle tissue recovery following exercise, which is necessary to prevent the progression of OA and maintain an independent, healthy lifestyle. The effects of omega-3 supplementation on the disease state of OA and its symptoms remain inconclusive. Further clinical trials utilizing human participants are warranted to provide a conclusive recommendation on standardized supplementation of omega-3 for the modulation of osteoarthritis.”
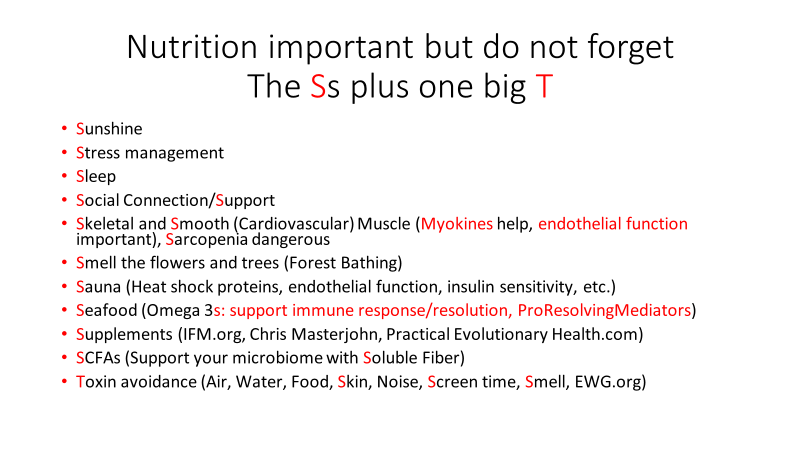
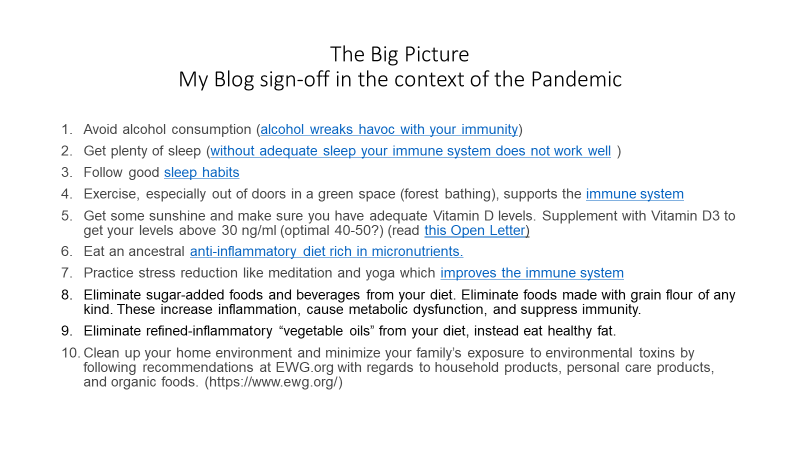
Given the cardioprotective effects, discussed in my last post (including an 80% reduction in sudden death at the highest quintile of omega-3 index) and other benefits (reduction in all cause mortality with high tissue levels), there are many reasons to include large amounts of low mercury fatty fish (wild Alaskan salmon, sardines, herring, trout) in the diet and to consider supplementation when your omega 3 index is < 8%. Likewise, in the presence of arthritis and pain, getting tissue levels of omega 3 up and reducing excessive pro-inflammatory omega 6 will likely provide significant benefit.
Here is a graphic with the omega 3 content of some foods.

And another:
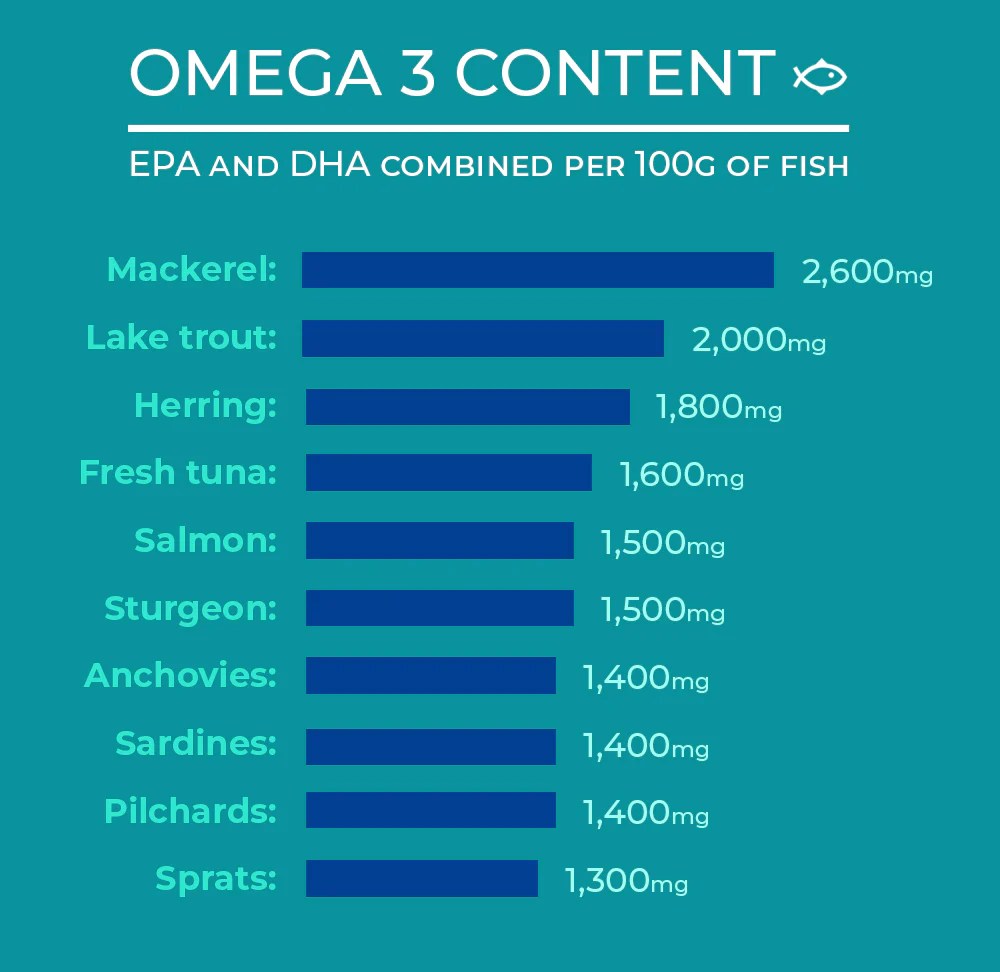
As mentioned in my previous post about omega-3 and cardiovascular health, 1800 mg of omega-3 FA daily is adequate in most people to achieve and omega-3 index of 8%, the level at which cardiovascular protection is greatest.
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob