I recently read an outstanding review of the topic “LONG COVID”. This has been defined in various ways. It can include persistent symptoms and/or organ damage following apparent “recovery” from the illness. There is no agreed upon definition. Our understanding is evolving. Time will tell how long symptoms can persist. It is clear that persistent symptoms and/or organ damage can occur even after minor illness or subsequent to asymptomatic positive PCR.
Full report can be found HERE
The following are EXCERPTS from the full report. References provided in the full report:
It has become clear in more recent months that an increasing number of individuals have been afflicted with persisting symptoms following a SARS-CoV-2 infection. Of these individuals, who have been referred to as “long-haulers” or as having “long COVID,” many did not initially experience a severe case of COVID-19, but rather had mild symptoms or were asymptomatic (Marshall, 2020)
According to Harvard Health, COVID-19 “long-haulers” include two groups of people affected by the virus (Komaroff, 2020):
· Those who experience some permanent damage to their lungs, heart, kidneys, or brain that may affect their ability to function.
· Those who continue to experience debilitating symptoms despite no detectable damage to these organs.
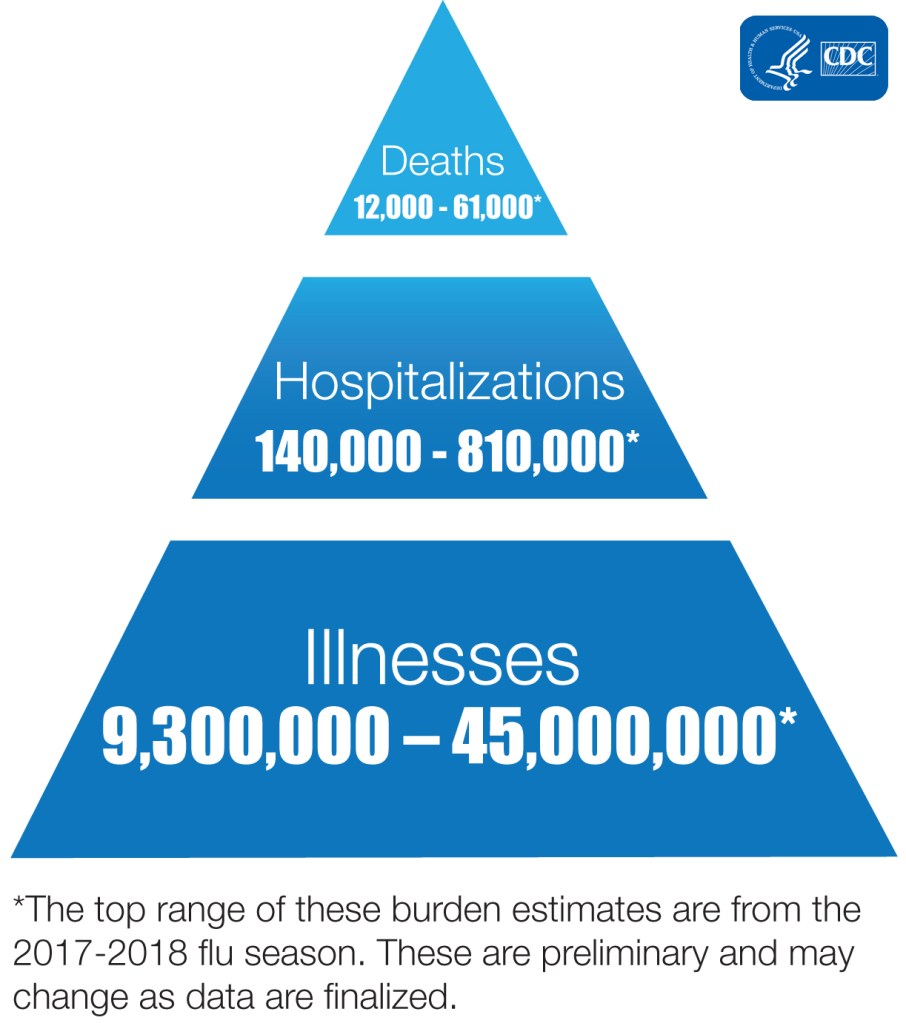
A team from the United Kingdom estimated that roughly 10% of individuals who have had COVID-19 experience prolonged symptoms (Greenhalgh et al., 2020). A guidance published on September 7, 2020 by Public Health England indicated that roughly 10% of “mild” COVID-19 cases who were not admitted to the hospital reported symptoms lasting more than four weeks (Public Health England, 2020).
Examples of some of the symptoms reported include:
· Prolonged low-grade fevers that do not respond to standard fever-reducing medications
· Neurological manifestations, such as memory loss and changes in the ability to recall words in a primary or secondary language
· Exercise-induced fatigue from walking around the block that led to a relapse of symptoms
· Symptoms in the central and peripheral nervous systems, gastrointestinal symptoms, skin problems, cardiovascular system occurrences
Some of the more commonly reported symptoms of long-COVID include: fatigue, cough, dyspnea, loss of taste and smell, muscle weakness, muscle and joint pain, headache, confusion, conjunctivitis, chest pain, decreased mobility and falls (Marshall, 2020; Paice et al., 2020).
On November 10th, 2020, the CDC updated its report entitled, “LongTerm Effects of COVID-19” (Centers for Disease Control and Prevention, 2020) to include the following information on long COVID: The most commonly reported long-term symptoms include:
· Fatigue
· Shortness of breath
· Cough
· Joint pain
· Chest pain
Other reported long-term symptoms include:
· Difficulty with thinking and concentration (sometimes referred to as “brain fog”)
· Depression
· Muscle pain
· Headache
· Intermittent fever
· Fast-beating or pounding heart (also known as heart palpitations)
More serious long-term complications appear to be less common but have been reported. These have been noted to affect different organ systems in the body. These include:
· Cardiovascular: inflammation of the heart muscle (in a German study 70% of patients had evidence of this, 80% of those patients had not been hospitalized)
· Respiratory: lung function abnormalities
· Renal: acute kidney injury
· Dermatologic: rash, hair loss
· Neurological: smell and taste problems, sleep issues, difficulty with concentration, memory problems
· Psychiatric: depression, anxiety, changes in mood
An organized study from Italy assessed the prevalence and types of persistent symptoms observed in 143 individuals after they were discharged from the hospital (Carfì et al., 2020)
The mean age of participants was 56.5 years old, with a range from 19 to 84 years of age, and 37% were female. The mean length of hospital stay was 13.5 days, and while in the hospital, 15% had received non-invasive ventilation, and 5% of the participants had received mechanical ventilation. The assessment described in the report occurred a mean 60.3 days after the onset of the first COVID-19 symptoms, and 12.6% were completely free of any virus related symptoms. The researchers reported that at a mean evaluation time of 60.3 days following COVID-19 symptom onset, 32% of the participants still had one to two symptoms, while 55% were still experiencing three or more symptoms.
The concept of chronic fatigue syndrome has been observed in individuals following infection with both viral and non-viral micro-organisms (Hickie et al., 2006). A study describing survivors of a SARS outbreak in Hong Kong stated that 40% had chronic-fatigue problems after three years and 27% met the criteria for chronic fatigue syndrome. The fatigue, also called postexertional malaise, results from a severe multi-organ crash following even light activities like a short walk. Similar effects have been reported after other large disease outbreaks (Hickie et al., 2006)
In summary, because the COVID-19 pandemic commenced only months ago, rather than years ago, the relatively long-term sequelae of COVID-19 are unknown; however, it seems that not unlike prior coronavirus outbreaks, COVID-19 has yielded reduced pulmonary and physical function, compromised quality of life and emotional distress. Unfortunately, prior outbreaks – including the SARS-CoV-1 epidemic — suggest that these associated effects can last for years (Marshall, 2020).
Challenges for people experiencing longer term effects from COVID19 can include:
· Widespread perception that people either die, get admitted to hospital, or recover after two weeks; however, it is clear that some individuals experience ongoing, or long COVID.
· Long COVID is a multisystem disease; thus, the symptoms vary significantly among the individuals with persisting effects from COVID19.
· It is unknown why some experience a prolonged recovery while others do not.
· Many individuals with mild or asymptomatic COVID-19 cases experience long-term COVID-19, but oftentimes, they were never initially tested for a SARS-CoV-2 infection, and therefore have not been flagged for a positive test result.
· There is a lack of consensus on diagnostic criteria for long COVID.
· Lack of guidance for reaching a working diagnosis and code for clinical datasets.
In the context of the COVID 19 pandemic I will close with the usual summary.
- Avoid alcohol consumption (alcohol wreaks havoc with your immunity)
- Get plenty of sleep (without adequate sleep your immune system does not work well )
- Follow good sleep habits
- Exercise, especially out of doors in a green space, supports the immune system
- Get some sunshine and make sure you have adequate Vitamin D levels.
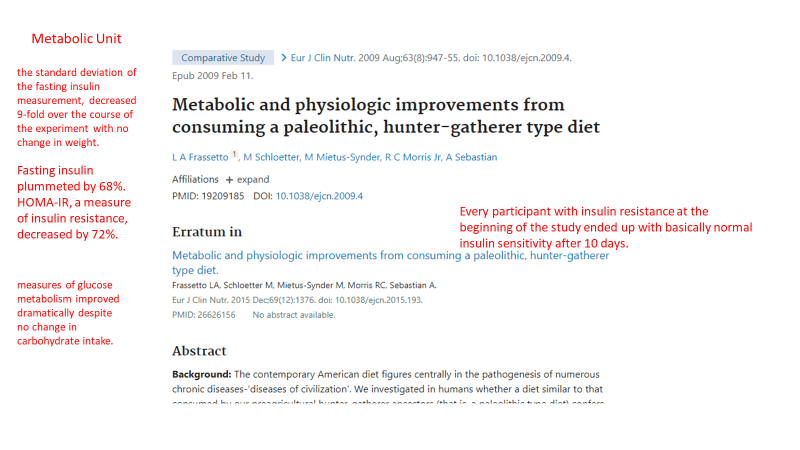
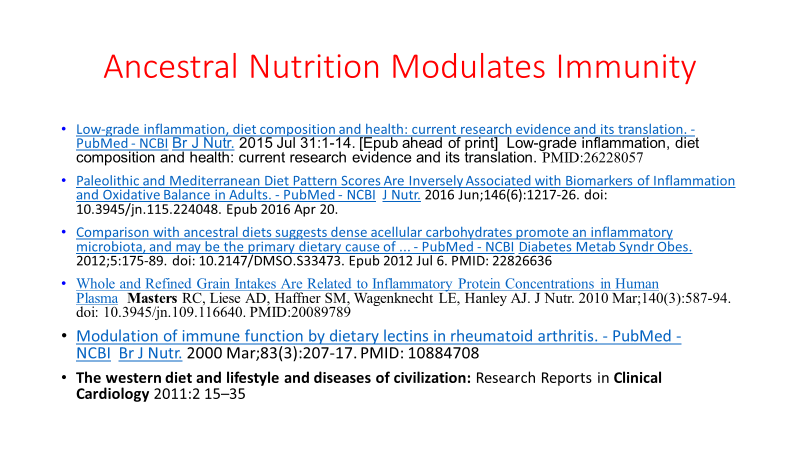
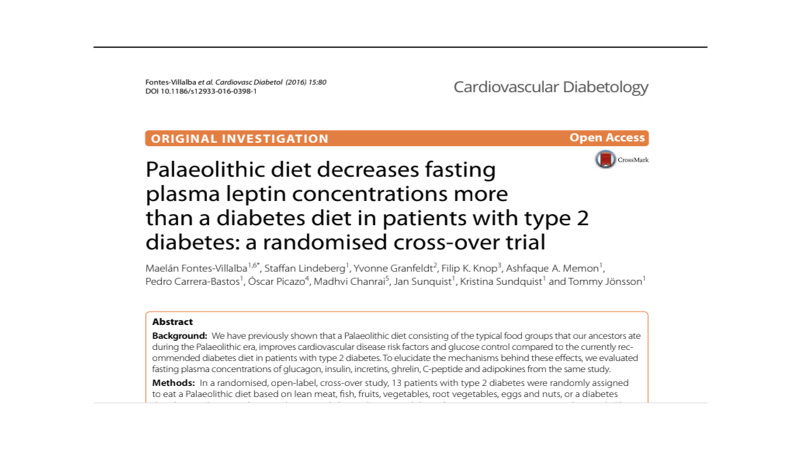
- Eat an anti-inflammatory diet rich in micronutrients.
- Practice stress reduction like meditation and yoga which improves the immune system
- Eliminate sugar-added foods and beverages from your diet. These increase inflammation, cause metabolic dysfunction, and suppress immunity.
- Eliminate refined-inflammatory “vegetable oils” from your diet, instead eat healthy fat.
- Clean up your home environment and minimize your family’s exposure to environmental toxins by following recommendations at EWG.org with regards to household products, personal care products, and organic foods. (https://www.ewg.org/)
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob