This discussion was originally posted before PAXLOVID WAS AVAILABLE. The title was originally Lifestyle More Effective than Drugs.
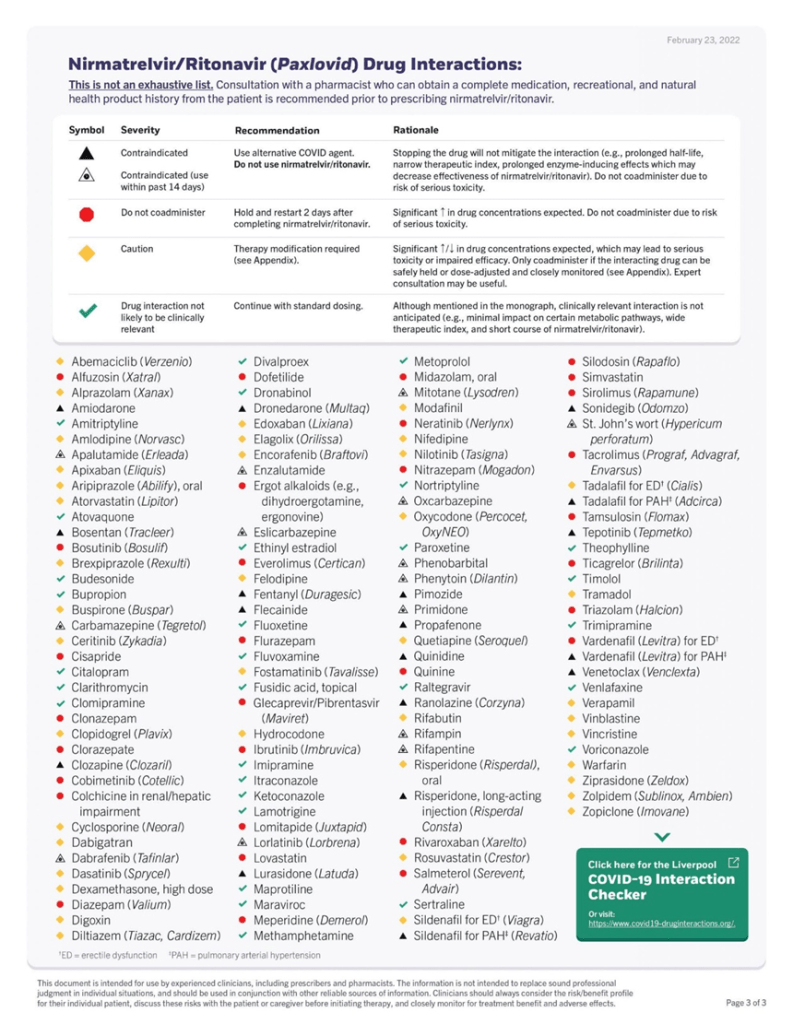
But now we have Paxlovid. Paxlovid is very effective in reducing morbidity and mortality associated with Covid-19 infection but also appears to reduce risk of Long Covid. Standard dosing: PAXLOVID two 150-mg tablets of nirmatrelvir, one 100-mg tablet of ritonavir twice daily for 5 days.
Dose adjustments are necessary for certain medical conditions and there are many drug interactions that should be considered. But do not let that discourage you from asking your provider to prescribe this drug for an acute Covid infection. This is a truly effective drug. It decreases morbidity and mortality as well as risk for Long Covid.
The results of a randomized placebo controlled clinical trial in high risk individuals has been published in the NEJM. The study was done just when Omicron hit. The study demonstrated an 89% reduction of hospitalizations and deaths by day 28 (absolute reduction of 6.2/100) with ZERO deaths in the Paxlovid group (7 in the placebo group). Paxlovid also had LESS side effects than placebo.
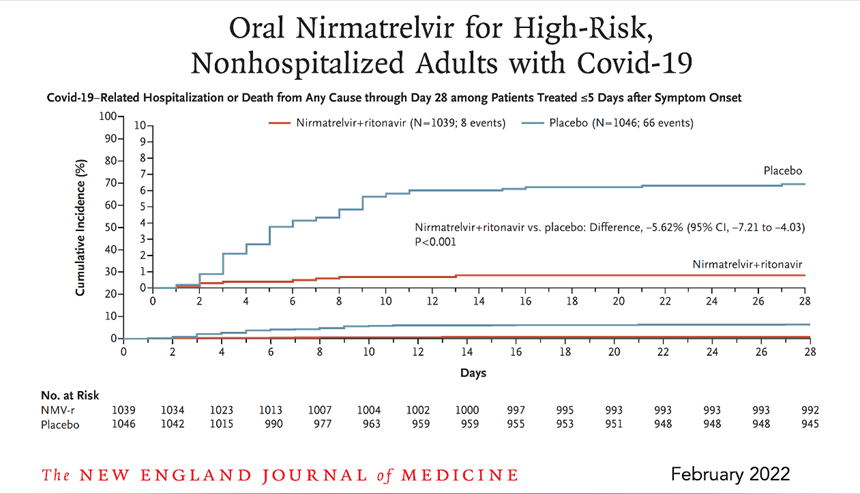
Another study from Israel demonstrated equally impressive results as shown here.
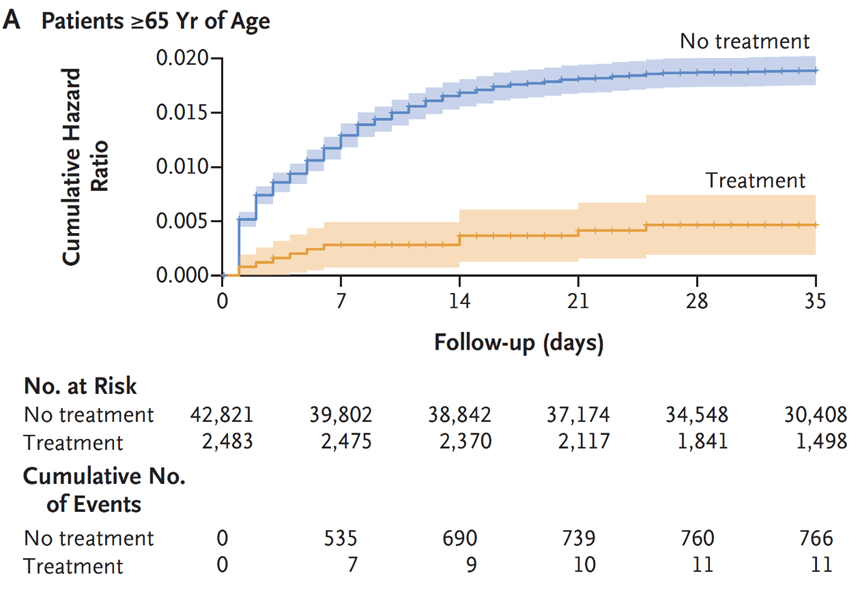
In addition, a study from the VA has looked at longer term effects (pre-print publication, still waiting for peer review.)
The study included 9000 Paxlovid patients treated within 5 days of symptom onset during the Omicron and subvariant waves and compared the treated patients with approximately 47,000 matched controls.
There was a 26% reduction in Long Covid.

Here is a breakdown of the Long Covid Symptoms

The VA study also showed a 48% reduction of death and 30% reduction in hospitalization after the acute phase (acute phase = first 30 days) as demonstrated here.

Many drug intervention trials for treating COVID-19 early in the pandemic have been disappointing. No studies have shown benefit for hydroxychloroquine, with or without azithromycin. This topic has been covered in previous posts. Remdesivir was FDA approved based upon one study that showed reduction in duration of symptoms. The mortality rate with Remdesivir, however, did not demonstrate a statistically significant difference when compared to “usual care”. https://www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19
Another study published in Lancet failed to show any clinical benefit from Remdesivir.
“No statistically significant benefits were observed for remdesivir treatment beyond those of standard of care treatment. Our trial did not attain the predetermined sample size because the outbreak of COVID-19 was brought under control in China. Future studies of remdesivir, including earlier treatment in patients with COVID-19 and higher-dose regimens or in combination with other antivirals or SARS-CoV-2 neutralising antibodies in those with severe COVID-19 are needed to better understand its potential effectiveness.”
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31022-9/fulltext
Likewise well designed studies of Ivermectin have shown no clinical benefit.
Monoclonal antibodies effective against early variants are no longer effective against the newer variants. So in terms of drug therapies for acute Covid infections we have Paxlovid for out patient care and dexamethasone for critically ill patients.
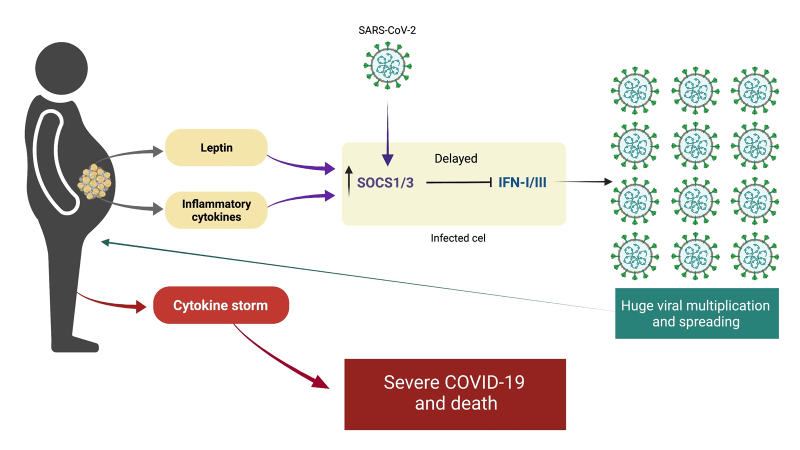
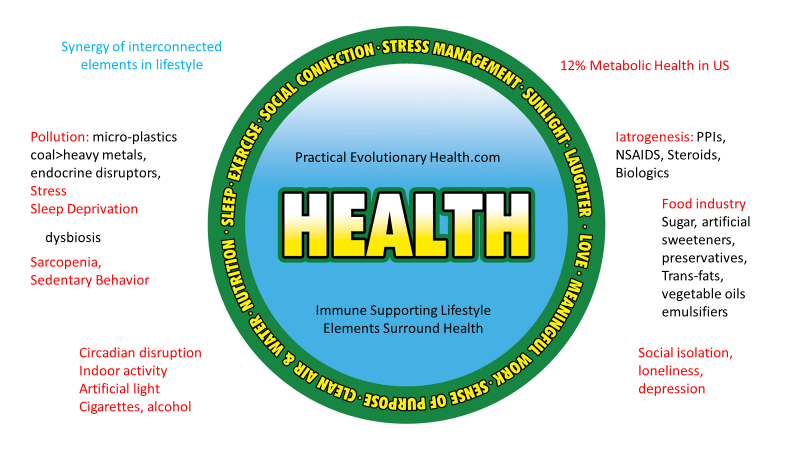
But we do know that certain underlying conditions such as obesity, diabetes, pre-diabetes (insulin resistance) and hypertension significantly increase risk of DEATH AND COMPLICATIONS with COVID-19. Since there are lifestyle interventions that can quickly and effectively mitigate these problems (diet, exercise, sleep, stress reduction….) now would seem like a good time to take our epidemics of obesity and diabetes in hand with aggressive lifestyle interventions to decrease the mortality rate of COVID-19 infection.
Such measures do not require expensive drugs or expensive drug trials, they simply require knowledge, guidelines and the will to implement change in our daily habits. Yet there has been little discussion about this in the media or on the part of public health officials.
Lets look at obesity in the US.
From 1999–2000 through 2017–2018, the age-adjusted prevalence of obesity increased from
30.5% to 42.4%, and the prevalence of severe obesity increased from 4.7% to 9.2%.
- Percent of adults aged 20 and over with obesity: 39.8% (2015-2016)
- Percent of adults aged 20 and over with overweight, including obesity: 71.6% (2015-2016)
- https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
The most effective tool for addressing obesity and diabetes is a very low carbohydrate diet.
Effects of the Low Carbohydrate, High Fat Diet on Glycemic Control and Body Weight in Patients With Type 2 Diabetes: Experience From a Community-Based Cohort
https://pubmed.ncbi.nlm.nih.gov/32193200/
This study was a done in a community-based program, not an academic practice setting. That is significant since it demonstrates feasibility outside of academic centers with standard community resources. The results of this study confirmed the results of many previous studies done in academic settings including better blood sugar control, reduction or elimination of diabetic medications, and significant weight loss.
“All patients following the LCHF diet who initially took
insulin had either a reduction or discontinuation of
this therapy by their healthcare provider when clinically
indicated, compared with less than a quarter of
those receiving usual care.“
In another study done in Italy, significant weight reduction (7 kg), waistline reduction (7 cm.), fat mass reduction (3.8%) and systolic blood pressure reduction (10.5 mmHg) were achieved in 3 months with a Very Low Carbohydrate diet.
Middle and Long-Term Impact of a Very Low-Carbohydrate Ketogenic Diet on Cardiometabolic Factors: A Multi-Center, Cross-Sectional, Clinical Study (https://pubmed.ncbi.nlm.nih.gov/25986079/
Nina Teicholz had an opinion piece published in the Wall Street Journal on May 30, discussing the USDA dietary guidelines that have largely ignored a massive body of evidence supporting a Very Low Carbohydrate Diet for obesity and diabetes. She cites many studies that have been ignored by the USDA dietary guidelines committee. Here is here opening statement.
“Americans with obesity, diabetes, heart disease and other diet-related diseases are about three times more likely to suffer worsened outcomes from Covid-19, including death. Had we flattened the still-rising curves of these conditions, it’s quite possible that our fight against the virus would today look very different.”
You can read the full article here:
https://www.wsj.com/articles/a-low-carb-strategy-for-fighting-the-pandemics-toll-11590811260
But think about that simple statement, THREE TIMES MORE LIKELY TO SUFFER WORSENED OUTCOMES FROM COVID-19. Yet these conditions are highly responsive to lifestyle interventions that not only mitigate obesity, insulin resistance and high blood pressure, but also enhance immune function.
More from Teicholz’s opinion piece:
“Other studies have found that dietary changes can rapidly and substantially improve cardiovascular risk factors, including conditions like hypertension that are major risk factors for worsened Covid-19 outcomes. A 2011 study in the journal Obesity on 300 clinic patients eating a very low-carbohydrate diet saw blood pressure quickly drop and remain low for years. And a 2014 trial on 148 subjects, funded by the National Institutes of Health, found a low-carb diet to be “more effective for weight loss and cardiovascular risk factor reduction” than a low-fat control diet at the end of the 1-year experiment.“
In a recent letter to the editor published in the journal METABOLISM, Dr. Casey Means points out:
A diagnosis of diabetes has been a key indicator of the severity of
COVID-19, and in this regard, the virus has relentlessly highlighted our
global Achilles heel of metabolic dysfunction, and points to a prime opportunity
to fight back.
That fight, however, is not going to be won with Clorox, Purell,
masks, or anti-IL-6 drugs. The fight will only be won through a serious
commitment to improving everyone’s foundational metabolic health,
starting with the lowest hanging evidence-based fruit: dietary and lifestyle
interventions.
Read the full letter here: https://www.metabolismjournal.com/article/S0026-0495(20)30118-9/pdf
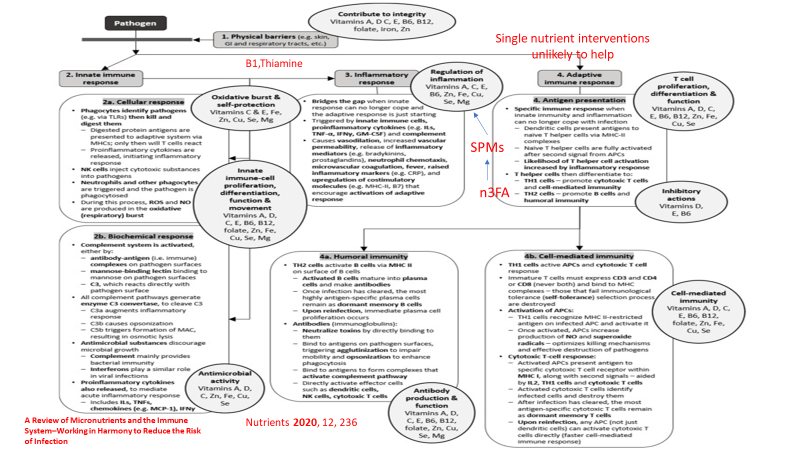
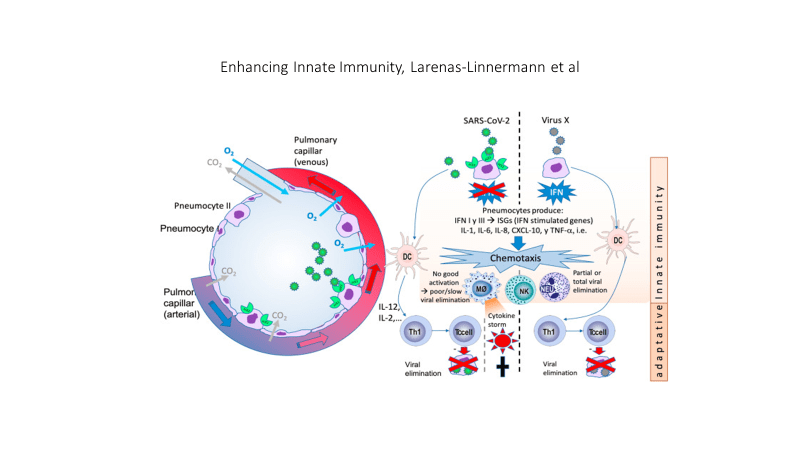
In 2 pages the letter describes multiple benefits of better glucose control relative to COVID -19 infection and the immune system as well as reduction of factors that lead to cytokine storm (terminal event for many COVID-19 patients). The letter also discusses the benefit of reducing environmental toxins (discussed in previous posts about COVID-19 and other health problems) that would likely benefit COVID-19 patients.
Research published April 18th, 2020 found that patients exposed to
highest amount of environmental nitrogen dioxide (NO2) had increased
risk of death fromCOVID-19, and that long-term exposure to this pollutant
may be one of the most important contributors to fatality by
compounding lung inflammation [20].
Minimizing exposure to environmental
pollutants may serve a role in quelling the underlying pro-inflammatory
state that characterizes metabolic disease and COVID-19 associated
cytokine storms.
Other environmental toxins, including persistent organic pollutants
(POPs) found in air, water, and food generated from pesticides
and industrial chemicals, are also strongly implicated in the pathogenesis
of metabolic syndrome; promoting “clean living,” toxin-avoidant
strategies for patients as simple as emphasizing organic foods, home
air purification, and non-toxic home supplies could be considered, although
the clinical utility of these measures in the acute setting is unknown
[21].
In discussing the white elephant in the room he states:
What is starkly missing is the clear, simple, and strong recommendation for no added
sugar or ultra-refined carbohydrates, both of which are known drivers
of postprandial hyperglycemia and inflammation. As a medical community, we must not miss the opportunity to serve patients with straightforward, evidence-based nutritional and lifestyle strategies to assist in glycemic control.
I would encourage you to follow the link and read the 2 pages supported by multiple peer-reviewed references.
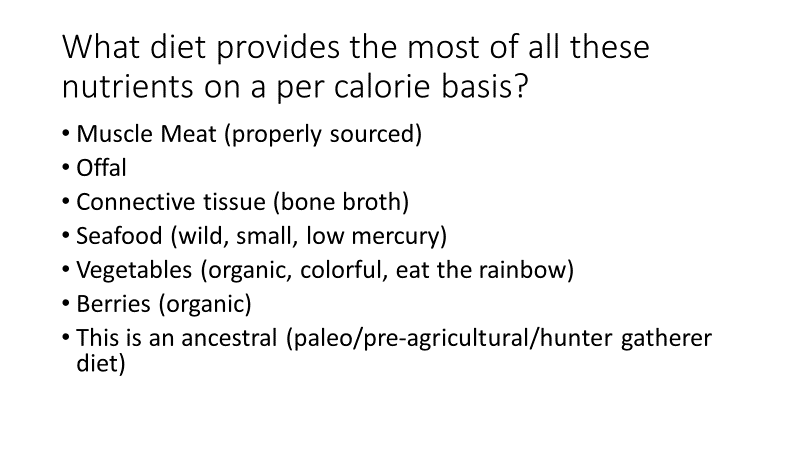
An ancestral (paleo) diet is also very effective for addressing insulin resistance, diabetes type 2 and obesity. Multiple studies have demonstrated this. Although an ancestral approach is typically low carb it is not typically ketogenic, but a ketogenic ancestral diet (high in non starchy vegetables to support the gut microbiome) can be implemented by restricting fruits to one serving of berries per day and limiting starchy vegetables.
Even without severe carbohydrate restriction, an ancestral anti-inflammatory diet will quickly address insulin resistance, type 2 diabetes, and obesity. In this study, insulin resistance was reversed in 10 days.

And another study compared an Ancestral (Paleo) diet to the Mediterranean diet in patients with ischemic heart disease AND insulin resistance (glucose intolerance or type 2 diabetes). Ancestral diet was superior to the Mediterranean diet in improving insulin sensitivity, blood sugar control and greater fat loss. Fasting blood sugars normalized in all patients on the Ancestral diet who had previously had abnormal blood sugars.

And here is a slide from one of my lectures with references on how an ancestral diet modulates immunity.
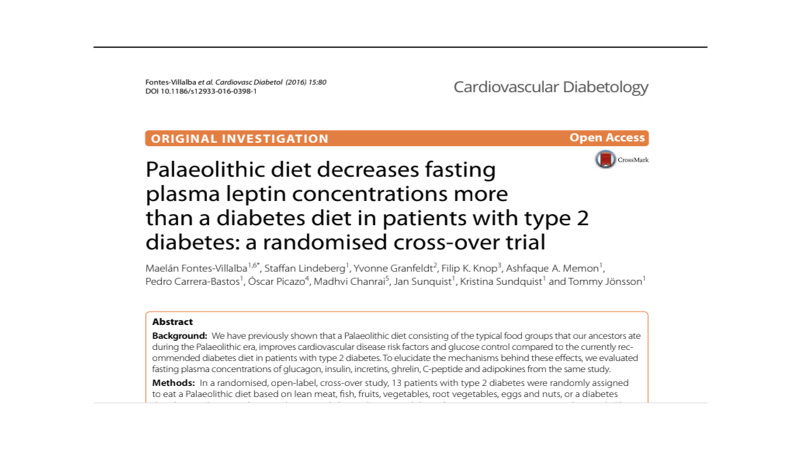
Leptin resistance, insulin resistance and obesity travel together. Here is yet another study demonstrating the effectiveness of an ancestral diet.
If you have obesity, diabetes or pre-diabetes the Very Low Carbohydrate version of the anti-inflammatory diet linked above would be the fastest and most effective intervention you can immediately employ to reduce your risk of succumbing to COVID-19. (Of course wear an N-95, follow good hygiene with hand-washing frequently, and use a HEPA filter or Corsi-Rosenthal box in your home, office, and enclosed work spaces)
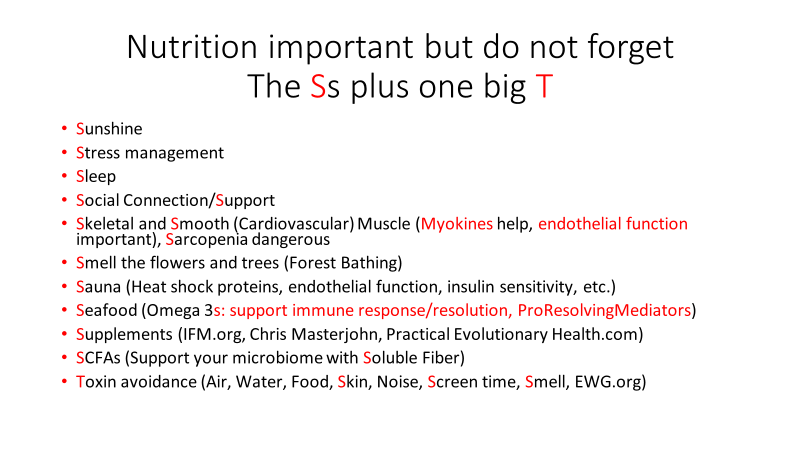
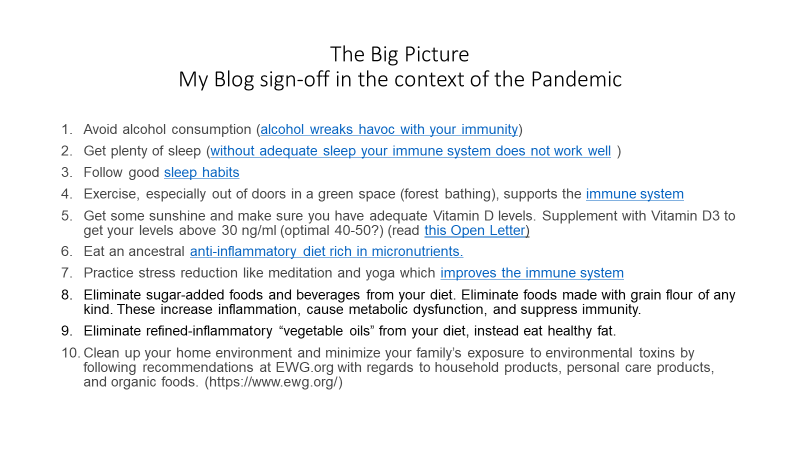
In the context of the COVID 19 pandemic I will close with the usual summary.
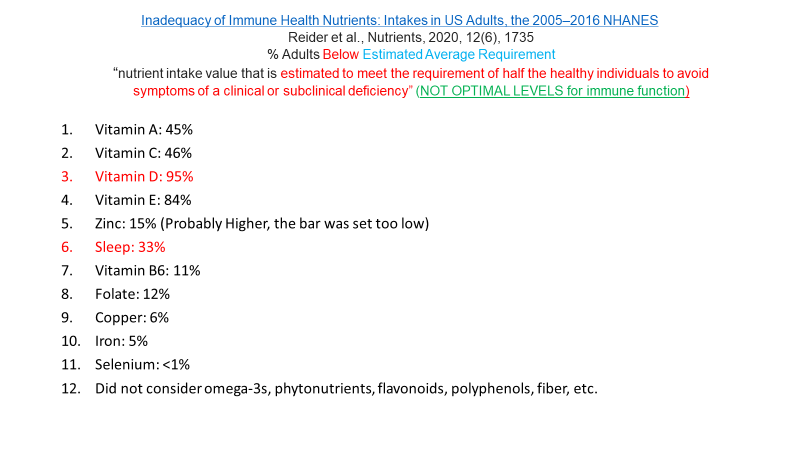
- Avoid alcohol consumption (alcohol wreaks havoc with your immunity)
- Get plenty of sleep (without adequate sleep your immune system does not work well )
- Follow good sleep habits
- Exercise, especially out of doors in a green space, supports the immune system
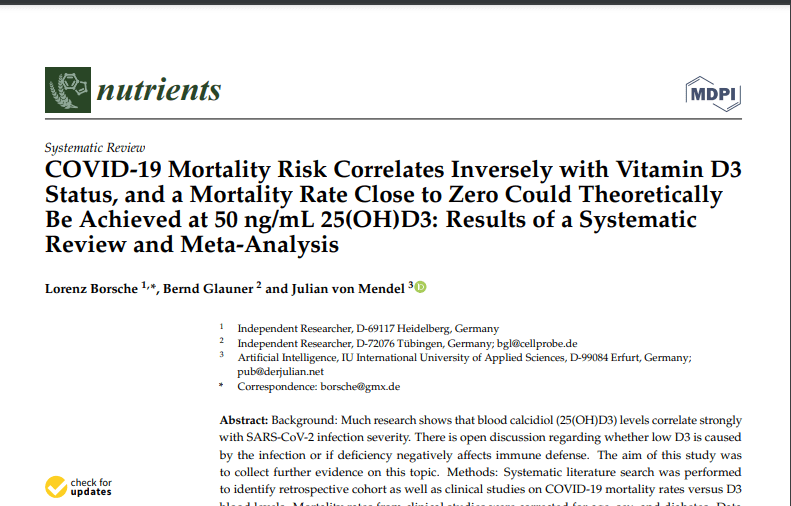
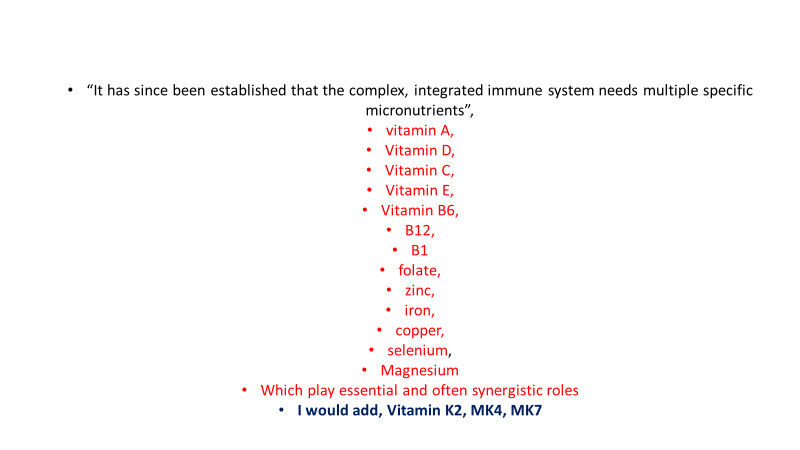
- Get some sunshine and make sure you have adequate Vitamin D levels. Supplement with Vitamin D3 to get your levels above 30 ng/ml, >40ng/ml arguably better.
- Eat an anti-inflammatory diet rich in micronutrients.
- Practice stress reduction like meditation and yoga which improves the immune system
- Eliminate sugar-added foods and beverages from your diet. These increase inflammation, cause metabolic dysfunction, and suppress immunity.
- Eliminate refined-inflammatory “vegetable oils” from your diet, instead eat healthy fat.
- Clean up your home environment and minimize your family’s exposure to environmental toxins by following recommendations at EWG.org with regards to household products, personal care products, and organic foods. (https://www.ewg.org/)
- Drink water filtered through a high quality system that eliminates most environmental toxins.
- HEPA filters or the home-made version (Corsi-Rosenthal box) used in your home or workplace can reduce circulating viral load as discussed on this website.
- If you are eligible for vaccination, consider protecting yourself and your neighbor with a few jabs. Age > 50 and/or risk factors (Diabetes, pre-diabetes, insulin resistance, hypertension, obesity, heart disease, COPD, asthma, cancer treatment, immune suppression) suggests benefit from a booster. Risk for complications of boosters in adolescents, especially males, without risk factors, may equal benefit. Previous infection with Covid can be considered as protective as a booster. Discuss risk vs benefits with your doctor.
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob