I was recently interviewed by a health blogger for his podcast. The topic was chronic inflammation. Here it is.
I prepared some notes for the interview. Here are the questions and answers.
What made you so interested in the topic of chronic inflammation?
Interest in chronic inflammation:
- Emerging evidence, source of most chronic disease including mental health (depression, etc.) is inflammation
- family health issues experience personally
- health care policy interest since graduate school
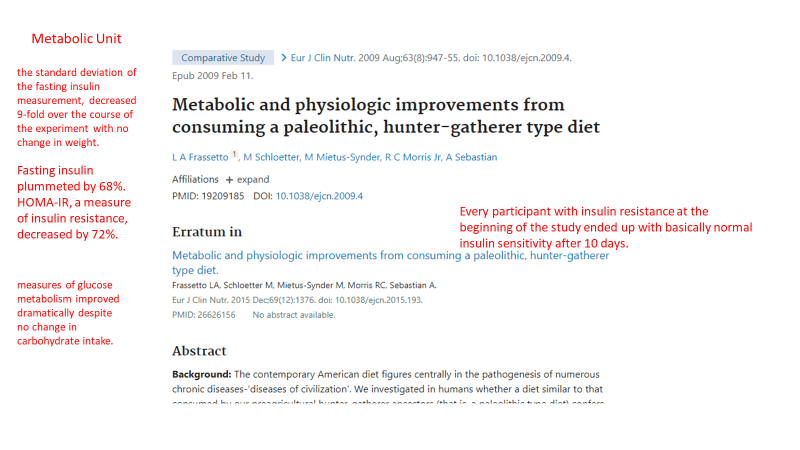
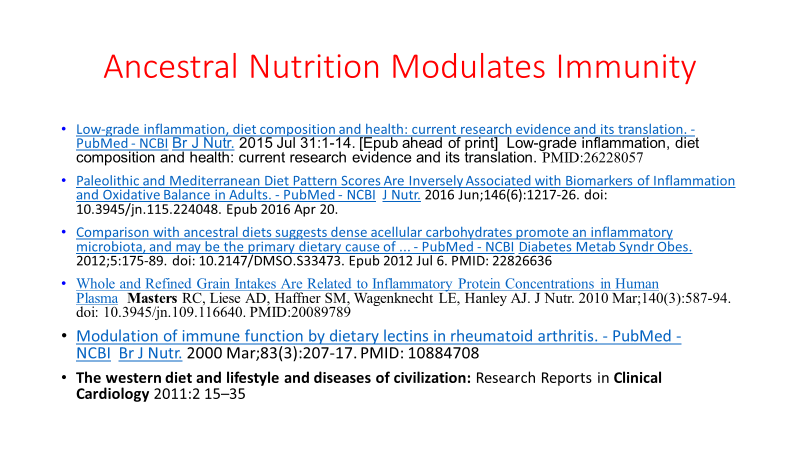
- First started to question USDA dietary advice after reading GOOD CALORIES, BAD CALORIES, by Gary Taubes,
- Experienced Statin myopathy, researched statin drugs, bad data, financial conflicts of interest. Sought alternative approaches to Coronary Artery Disease prevention.
- In USA, Profit driven health care system evolved from more benign not-for-profit earlier system in medical insurance and hospital system. Drug and surgery oriented. Corporate ownership of multiple hospitals, concentration of wealth and power in the industry and in society in general
- Saw this every day: growing obesity, Metabolic Syndrome, DMII, auto-immune disease. Root causes NOT ADDRESSED.
- While recovering from surgery attended on line functional medicine conference on auto-immune disease, covering diet, sleep, exercise, sunshine, Vitamin D, environmental toxins, gut dysbiosis, intestinal permeability (THE GATEWAY TO AUTOIMMUNITY IS THROUGH THE GUT).
- Introduced to EVOLUTIONARY BIOLOGY and Paleo Diet by my son
What diseases does chronic inflammation typically lead to?
- Cancer
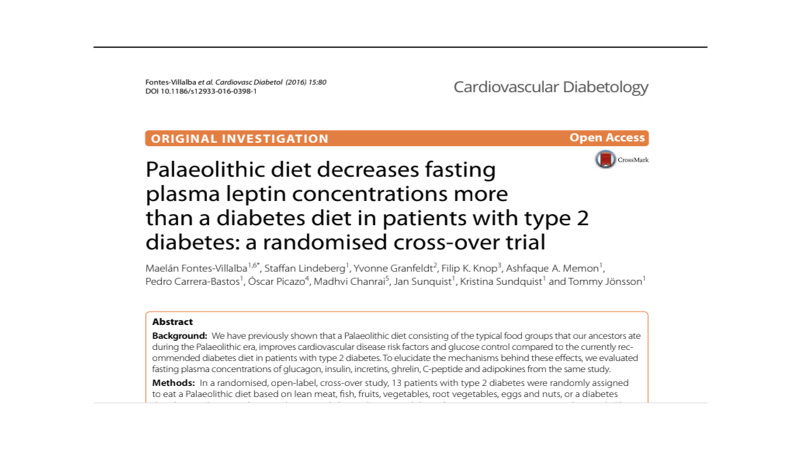
- Diabetes
- Obesity epidemic, DIABESITY
- Hypertension
- Metabolic Syndrome (3/5: HTN, insulin resistance/high blood sugar, abdominal obesity, high TGs, low HDL),
- Autoimmune diseases
- Degenerative arthritis
- Neurodegenerative disorders (dementia, Parkinson’s, neuropathy, multiple sclerosis)
- Works of Dale Bredesen (dementia, “The End of Alzheimer’s”), Ron Perlmutter (Grain Brain), Terry Wahls (The Wahls protocol for MS), all FUNCTIONAL MEDICINE looking at root cause of illness, common-overlapping threads.
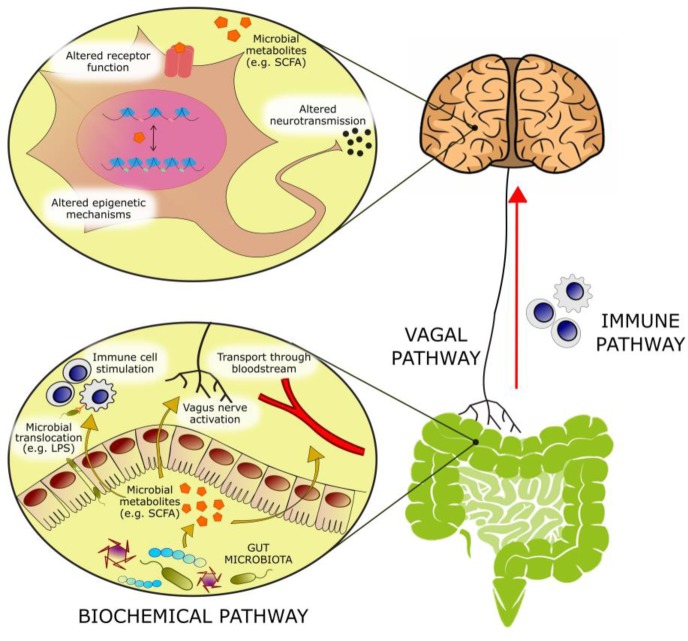
- Interplay between sleep, circadian rhythm, exercise, sunlight, stress, environmental toxins, diet, processed foods, nutritional deficiency, gut microbiome, endocrine disruptors, intestinal permeability, oral and skin microbiome, social disruptors, GUT BRAIN AXIS. These are all part of one large ECOSYSTEM.
- Positive and negative feedback systems requiring a SYSTEMS ENGINEERING approach to understanding root causes.
- Butyrate is the preferred substrate for colonocytes, providing 60-70% of the energy requirements for colonic epithelial cells1,2. Butyrate suppresses colonic inflammation,3 is immunoregulatory in the gut,4 and improves gut barrier permeability by accelerating assembly of tight junction proteins.5,6
- Improves insulin sensitivity, increase energy expenditure, reduce adiposity, increases satiety hormones,
- HDAC activity inhibitor, PROTECTS GENES from removal of necessary acetyl groups.
- Butyrate also influences the mucus layer. A healthy colonic epithelium is coated in a double layer of mucus. The thick, inner layer is dense and largely devoid of microbes, protecting the epithelium from contact with commensals and pathogens alike. The loose, outer layer of mucus is home to many bacteria, some of which feed on the glycoproteins of the outer mucus layer itself. Both of these mucus layers are organized by the MUC2 mucin protein, which is secreted by goblet cells in the epithelium. Supplementation of physiological concentrations of butyrate has been shown to increase MUC2 gene expression and MUC2 secretion in a human goblet cell line.7,8
What are the population groups which have higher risk of chronic inflammation?
- Obese
- Sedentary
- Poor-urban-polluted environment dwelling (air, water, noise, crowding, violence, racism, oppression)
- Divergence from ancestral evolutionary biology
- Working environment: indoors, polluted, oppressive supervisors, no sunlight, noise pollution, air pollution, toxic social situations, repetitive motion, bad ergonomics,
- night shift, disruption of circadian rhythm
- both parents working, no time for real food and family interaction, supervision of children.
- screen time- sedentary behavior, lack of outdoor activity
- Stress of social inequality, food insecurity, violent neighborhoods, nutritional deserts
What are the “danger signs” or typical symptoms which may signal a chronic inflammation?
DANGER SIGNS:
- Waistline (waist to height ratio, BMI)
- Sarcopenia (muscle as an endocrine organ)
- Sleep disturbance
- Pain
- Headaches
- Depression
- Lack of joy.
- Brain fog, fatigue
What are the typical biomarkers of chronic inflammation?
- METABOLIC SYNDROME (3 or more of the following: high blood pressure, elevated blood sugar, elevated Triglycerides, low HDL, obesity)
- CRP predictive of cardiovascular events,
- ESR associated with arthritis
- Stress hormones (morning cortisol levels)
- Resting Heart Rate and Heart Rate Variability
What are the typical sources of systemic chronic inflammation?
Sources of Chronic Inflammation:
Diet
- N6/N3 FA ratio determined by too much Refined Easily Oxidized Vegetable Oils, not enough marine sources of N3 FA, grain fed vs grass fed/finished ruminant meat. Loren Cordain research wild game FA composition = grass fed. Margarine vs Butter. Fried foods using Vegetable oils. Oxidized fats/oils, oxy-sterols in diet.
- Sugar excess leading to insulin resistance
- Refined carbs leading to insulin resistance (dense acellular….)
- Disturbance of gut microbiome from poor nutrition (sugar, refined carbs and vegetable oils all disrupt the microbiome)
- Gut brain axis.
- Food ADDITIVES AND PRESERVATIVES
- Trans Fats (finally banned)
Endocrine disruptors/ BIOACCUMULATION
- Plastics (microparticles in our fish, food and bottled water)
- Plastic breakdown products
- Phthalates added to plastics to increase flexibility ( also pill coatings, binders, dispersants, film formers, personal care products, perfumes, detergents, surfactants, packaging, children’s toys, shower curtains, floor tiles, vinyl upholstery, it is everywhere) 8.4 million tons of plasticizers produced annually. EWG.org
- Pesticides, herbicides, glyphosate (Monsanto), DIRTY DOZEN, CLEAN FIFTEEN EWG.org
- Medications
- ABSORBED skin, eat, drink, breath,
- BPS is as bad as the BPA it replaced
- Polychlorinated biphenyls used in INDUSTRIAL COOLANTS AND LUBRICANTS
- Flame retardants (PBDEs, polybrominated dipheyl ethers) are ubiquitous in furniture and children’s clothing. Also linked to autoimmune disease
- Dioxins
- PAHs (polycyclic aromatic hydrocarbons
- Sunblock
- CUMULATIVE BURDEN, INTERACTIONS, SYNERGY?
SLEEP DEPRIVATION CHRONIC IN OUR SOCIETY
Eating late vs time restricted eating
Gut Microbiome disrupted by
- 1/3 of prescribed medications disrupt the microbiome AND increase intestinal permeability
- Stress
- Sleep deprivation
- Sugar
- Refined carbs
- Refined veg oils
- Over exercise and Under exercise, both are bad.
- Environmental toxins
Gut dysbiosis and infections include (often chronic, low grade, not diagnosed)
- Pathogenic bacteria, infection or overgrowth/imbalance
- SIBO
- Parasites
- Viruses
- BAD bugs > good bugs
- Good bugs make vitamins and SCFAs required for colonocyte energy
- Gut-Brain axis huge topic, VAGUS NERVE COMMUNICATION both ways, SCFA in gut and in CIRCULATION (butyrate, propionate, acetate), NEUROTRANSMITTER PRODUCTION (SEROTONIN, OTHERS), enterochromaffin cells producing > 30 peptides.
- Overuse of antibiotics in medicine
- AND use of antibiotics in raising our food.
- Vaginal delivery vs C-section
- Breast feeding vs bottle feeding
INCREASED INTESTINAL PERMEABILITY:
- Caused by all factors above
- Leads to higher levels of circulating LPS-endotoxin, bacterial products that create an immune-inflammatory response.
- Incompletely digested proteins with AA sequences overlapping our own tissue causing autoimmunity/inflammation through molecular mimicry
Heavy Metal toxicity
- Lead
- Mercury
- Cadmium
- Arsenic
MOLD TOXICITY (> 400 identified mycotoxins, can cause dementia, asthma, allergies, auto-immunity)
- At home
- At work
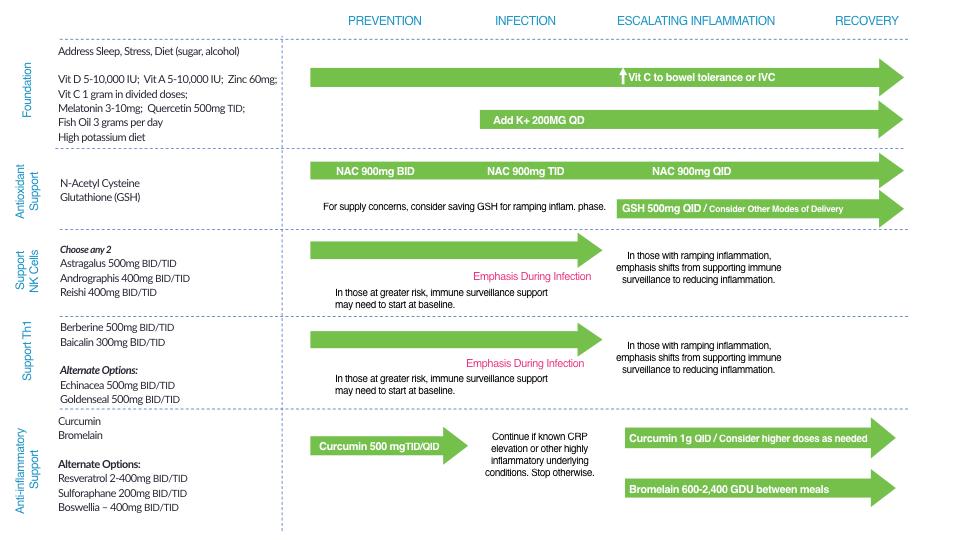
What are the most efficient natural (non-medication) ways to address chronic inflammation?
- Anti-inflammatory Diet, real whole food that our ancestors ate through evolutionary history (grass fed/finished ruminant meat, free range poultry, antibiotic free, and pesticide free food, wild seafood (low mercury varieties), organic vegetables and fruit, nuts, fermented foods, eggs)
- Low mercury fish and seafood for omega three fatty acids
- Sleep hygiene
- Exercise, not too much, not too little, rest days, out of doors, resistance training, walking, yoga, Pilates, tai chi, chi gong, dancing, PLAYING!!!!!!!!!!!!!
- Stress reduction: meditation, mindful living, forest bathing, sunlight, Playing, music, praying, SOCIAL CONNECTION, laughter, comedy, quit the toxic job, quit the toxic relationship, SAUNA/SWEAT, heat shock proteins, exercise
- Vitamin D, sunshine, check levels
- PLAY, PLAY, PLAY, LAUGH, DANCE, ENJOY, LOVE
- Be aware of potential dangers of EMF, WiFi, hand held devices, blue tooth headphones.
- Address environmental justice
- Address social inequality, food insecurity
- Tobacco addiction
- Ethanol
- Other substance abuse
- Agricultural subsidies in US distort the food supply
- Loss of soil threatens food supply
- Suppression of science (global warming, environment, etc.,) worsens environmental degradation, creating an EXISTENTIAL THREAT.
- Avoid alcohol consumption (alcohol wreaks havoc with your immunity)
- Get plenty of sleep (without adequate sleep your immune system does not work well )
- Follow good sleep habits
- Exercise, especially out of doors in a green space, supports the immune system
- Get some sunshine and make sure you have adequate Vitamin D levels.
- Eat an anti-inflammatory diet rich in micronutrients.
- Practice stress reduction like meditation and yoga which improves the immune system
- Eliminate sugar-added foods and beverages from your diet. These increase inflammation, cause metabolic dysfunction, and suppress immunity.
- Clean up your home environment and minimize your family’s exposure to environmental toxins by following recommendations at EWG.org with regards to household products, personal care products, and organic foods. (https://www.ewg.org/)
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob