This is an excerpt from a MEDSCAPE article. MEDSCAPE is a clinical on-line source of information.
“Clinicians across the United States are petitioning the federal government to follow the lead of South Korea, China, and other nations by imposing an immediate nationwide quarantine to slow the inevitable spread of COVID-19. Without federal action, the creators say, their lives and the lives of their colleagues, patients, and families are being put at increased risk.
In addition to the quarantine, the petition, posted on the website Change.org, calls on US leaders to institute emergency production and distribution of personal protective equipment for healthcare workers and to rapidly increase access to testing.
The petition, which garnered more than 40,000 signatures in just 12 hours and as of this writing was approaching 94,000, was started by an apolitical Facebook group to focus attention on what members see as the most critical issues for clinicians: slowing the spread of the virus through a coast-to-coast quarantine; protection of medical personnel with adequate supplies of essential equipment; and widespread testing.”
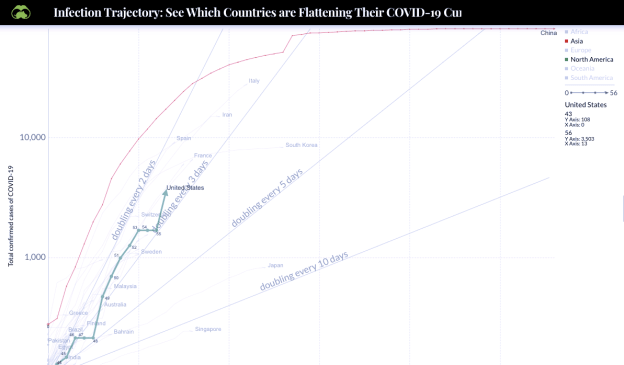
Meanwhile, growth curves for various countries show US is on the same path as ITALY. The doubling time of cases in the US appears to be about 2 days! See the slope for the US on the chart below. Compare it to the double-every-2-day line.
You can see the direct source of this curve here. But on the curve below the US has been superimposed. (added) Please note that # cases is on a logarithmic scale.
Doctors at the front line are trying to protect everyone, including their own families who are at risk from their daily exposure while at work.
“The COVID-19 US Physicians/APP Facebook group includes 20 volunteer moderators who handle hundreds of posts per hour from persons seeking information on the novel coronavirus, what to tell patients, and how to protect themselves.”
While initially denying the problem, CHINA subsequently took drastic measures and the results are evident in the curve above. Almost complete cessation of growth has occurred in China (but this could rebound as restrictions are removed).
China is not an open society and personal freedom, that we cherish so dearly and appropriately defend, in combination with ineffective leadership, has produced the deadly and alarming situation in the US.
The response in the US has been TOO LITTLE, TOO LATE.
Finger pointing at this critical time will distract from our country uniting to fight this. But we need thoughtful and effective leadership at the highest level, which has been tragically lacking.
At the same time we must learn from our mistakes and the mistakes of others.
“When health authorities in Wuhan, China ― widely cited as the epicenter of the global pandemic ― cordoned off the city, the infection rate dropped from one person infecting 3.8 others to one infecting 1.25, thereby significantly slowing the rate of transmission.”
Early on, WHO-approved test kits (made in Germany) were available but the US did not use them and instead waited for kits to be produced in the US. (Whitehouse mandate) Our testing is still FAR behind other countries, delaying a full scale response.
Doctors from around the country have reported shortages of test kits and PPE (sources: personal phone calls to my colleagues across the country, various press reports, and The COVID-19 US Physicians/APP Facebook group)
The present administration eliminated, soon after taking office, the Pandemic Emergency Response Team that would have coordinated multiple Federal Agencies responding to a PANDEMIC.
Why? “Unnecessary duplication”.
If a centralized coordinating TEAM was not necessary why are we seeing such an ineffective response to the crisis (rapid growth rate of cases)?
Hospitals in hot zones will soon be running short on masks, gloves, gowns (PPE, personal protection equipment) that protect health workers from contracting the disease. Previous OSHA rules would have required (before COVID-19 existed) that hospitals stockpile these supplies in adequate amounts to meet the demands of a PANDEMIC. This measure was tragically removed from OSHA requirements by the present administration. (too expensive)
We must stop making mistakes and respond forcefully, quickly, more intensely and learn from these and other mistakes to avoid this in the future.
So think about the petition signed by 94,000 (and growing) US doctors and other providers which asks for an immediate coast to coast quarantine and immediate emergency-funded production/distribution of PPE and test kits.
White House press conferences have promised allot but produced very little. Germany has ordered 10,000 new ventilators and asked a manufacturer to immediately increase production. The Whitehouse, after stating that “many, many ventilators” would be available later told governors to fend for themselves in getting ventilators. (no instructions for where/how were provided)
Because we have, as a nation, done too little too late, we must now take EVEN MORE drastic measures. We must unite, cooperate, and listen to the doctors and nurses on the front lines (as described in the petition).
Last week FOX NEWS was still describing COVID-19 as less serious than the flu! Apparently they have thankfully started to change their tune.
BEWARE OF FAKE NEWS.
Here is a comparative chart by country. Please note that # cases is on a logarithmic scale..
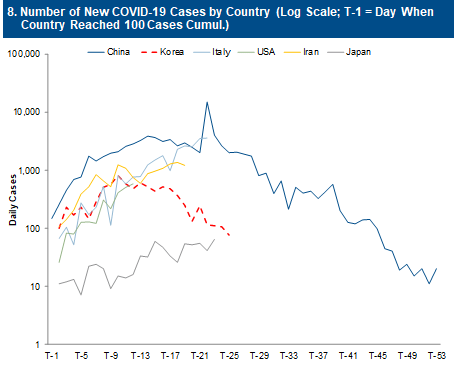
This shows how South Korea quickly flattened the curve with fast and effective action while the US continued to demonstrate rapid rates of growth. South Korea instituted major closures, shelter-in-place, and widescale rapid testing. South Korea responded appropriately with strong and effective leadership. South Korea is much closer to the original source and has as much international travel as the US.
US citizens must think and act responsibly and listen to the petition of >94,000 doctors and other providers.
Yesterday’s Bay Area testing was 1700 total tests, 55 positives. About 3%. This ties with the Wuhan rate before drastic measures were instituted.
STAY AT HOME except for essential items and urgent medical care. Do not travel. If you have any symptoms self-quarantine. Follow home hygiene recommendations. Go to the CDC website for details on protection..
Here are some other CDC links
Are You at Higher Risk for Severe Illness?
All A-Z TopicsCoronavirus Disease 2019 (COVID-19)
In my rural county there has only been one case reported (a traveler who returned home) but this is the tip of the iceberg here and testing has not been widespread. Although compared to other areas our Department of Public Health states we are still low risk it is only a matter of days or weeks before that changes. The risks increase on a daily basis EVERYWHERE. Rural areas are just a week or two behind major cities.
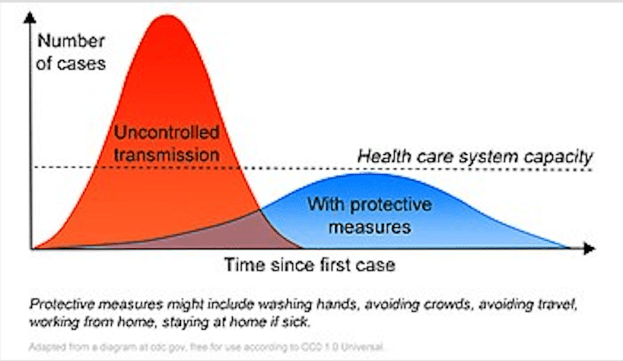
We must all do our part to flatten the curve.
Please share this discussion widely with friends, family and colleagues.
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob