This video, produced by a colleague, is very informative.
Sleep well, exercise outdoors, laugh, love, engage in meaningful work, drink filtered water, eat clean, eat whole foods, get plenty of sunshine, spend time with those you love.
Doctor Bob
This video, produced by a colleague, is very informative.
Sleep well, exercise outdoors, laugh, love, engage in meaningful work, drink filtered water, eat clean, eat whole foods, get plenty of sunshine, spend time with those you love.
Doctor Bob
A report from the Imperial College in UK summarizes the results of a model utilizing the most up to date data available. Very sobering!!
Some key points.
We find that that optimal mitigation policies (combining home isolation of suspect cases, home quarantine of those living in the same household as suspect cases, and social distancing of the elderly and others at most risk of severe disease) might reduce peak healthcare demand by 2/3 and deaths by half.
However, the resulting mitigated epidemic would still likely result in hundreds of thousands of deaths and health systems (most notably intensive care units) being overwhelmed many times over.
For countries able to achieve it, this leaves suppression as the preferred policy option.
We show that in the UK and US context, suppression will minimally require
The major challenge of suppression is that this type of intensive intervention package – or something equivalently effective at reducing transmission – will need to be maintained until a vaccine becomes available (potentially 18 months or more) – given that we predict that transmission will quickly rebound if interventions are relaxed.
We show that intermittent social distancing – triggered by trends in disease surveillance – may allow interventions to be relaxed temporarily in relative short time windows, but measures will need to be reintroduced if or when case numbers rebound
Last, while experience in China and now South Korea show that suppression is possible in the short term, it remains to be seen whether it is possible long-term, and whether the social and economic costs of the interventions adopted thus far can be reduced.
Certainly this is very sobering. We are in this for the long haul. Reports of some beneficial effects of drugs presently used for other purposes are providing hope for the critically ill.
Various cities and counties have instituted curfews and local ordinances, closing non-essential business under penalty of criminal charges. These measures are necessary for immediate mitigation and suppression.
San Francisco instituted a “shelter in place” starting at 12:01am this morning in order to enforce enhanced social distancing measures. Again, a wise measure in a hot zone.
Anthony Fauci MD, Director of Infectious Disease and Allergy at NIH has sated “if someone tells you that you are over-reacting then you are doing it right”.
“Younger people should be concerned for two reasons. You are not immune or safe from getting seriously ill. Even though when you look at the total numbers, it’s overwhelmingly weighted toward the elderly and those with underlying conditions. But the virus isn’t a mathematical formula. There are going to be people who are young who are going to wind up getting seriously ill.
So protect yourself, but remember that you can also be a vector or a carrier. And even though you don’t get seriously ill, you could bring it to a person, who could bring it to a person, that would bring it to your grandfather, your grandmother or your elderly relative. That’s why everybody has to take this seriously, even the young.”
Too many in our community are under-estimating the gravity of this situation and the measures necessary to save lives. Those who ignore these recommendations increase risk for their families, friends, and society at large.
Stay at home except for necessities which include food, medicines, urgent medical care.
Immediately wash your hands with soap and water for at least 20 seconds when you come home or come in contact with anything from the outside. Soap and water more effective than hand sanitizer.
Wipe down hard surfaces with Clorox type disinfectants in kitchen, bathroom, phone, door knobs, car door handles, steering wheels, etc.
When out in public for necessities wear gloves, eye protection. Disinfect shopping cart handles before touching them AND wear gloves.
Any item brought into the home handled by other folks should be wiped with disinfectants.
Wash clothing and sheets frequently. Droplets from asymptomatic carriers of COVID-19 can remain on clothing and hard surfaces for a few days and remain infectious. If a retail worker touches their face then touches the item you purchase (or coughs or sneezes on an item) it could transmit disease.
Keep your immune system optimal:
Stay safe.
Sleep well, exercise outdoors, laugh, love, engage in meaningful work, drink filtered water, eat clean, eat whole foods, get plenty of sunshine, spend time with those you love.
Doctor Bob
Here is the link to a great interactive tool that shows the risk reduction or increase with early/aggressive vs. late/mild intervention with respect to social distancing etc. I highly recommend visiting this site. You can move the time line through various scenarios. The site also provides very useful information. Hat tip to my friend Joe Andresen MD for sending me the link.
Be Safe.
Doctor Bob
Here it is, you can subscribe to receive daily email update.
Stay safe.
We are past the point of containment, COVID19 is here. A travel ban from Europe (announced by Trump) is useless. It will cause harm by diverting resources from truly effective measures. Yes, travel bans cost money and resources to implement, money and resources better spent elsewhere.
Experts advise that we must flatten the curve of COVID19 spread to prevent overwhelming our medical facilities and personnel. The US has a finite number of ICU beds, hospital beds, doctors, nurses and technicians. In fact the number of hospitals and hospital beds has dropped considerably compared to other countries.
FROM MSN:
“The limits of America’s hospital system are an unexpected downside of progress in efficiency, advances in technology and pharmaceutical breakthroughs that have made it easier to keep patients out of the hospitals. Insurers have accelerated the trend by steering patients to less-costly care, pushing for more procedures to be done on an outpatient basis, often outside hospital walls. The number of hospital beds—and hospitals—has contracted in recent decades, dropping 16% and 12%, respectively, between 1975 and 2018, according to survey data from the American Hospital Association.
After years of consolidation and scaling back on construction, with the sector pouring more capital into outpatient centers, the system has less capacity for surges in demand.
U.S. hospital beds per American have declined in the past two decades to a ratio of 2.8 beds for every 1,000 people as of 2016. That ranks among the lowest across comparable countries, a Kaiser Family Foundation analysis of Organization for Economic Cooperation and Development data shows. The average across those countries, including Japan, Germany and Australia, is 5.4 beds per 1,000 people.”
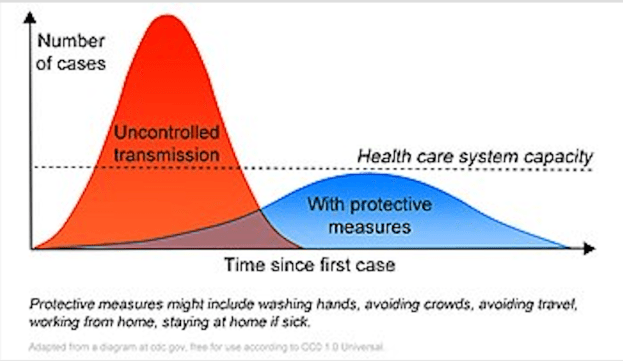
So what does it mean to “flatten the curve?
We must take measures that will slow down the rise of cases and flatten the peak so that our resources can handle a lower and more widely spread peak. There will be a critical point where if more sick cases appear not everyone will get the care they need (no more ventilators, no more ICU beds, etc.) That point is represented by the Health care system capacity line below.
SOCIAL DISTANCING:
Social distancing includes avoiding crowded spaces such as theatres, museums, concerts, public gatherings. What size constitutes a “crowd”? The cutoff is arbitrary. The NBA and NHL have canceled their seasons. NYC has closed museums and Broadway theatres are closed. More stringent social distancing closes smaller venues. This sort of activity requires effective leadership which presently is coming from states and local governments. (Trump has failed to lead us. He has ignored and contradicted expert opinion from CDC etc. More about that another time.)
OTHER MEASURES:
As indicated in the above graph depicting flattening the curve, we as individual citizens can help flatten the curve.
Many people do not have paid sick time. That is why immediate federal legislation to support sick people so they can stay home is vitally important. That leadership is thankfully coming from Nancy Pelosi.
FROM NPR: “House Speaker Nancy Pelosi says her chamber will move forward Friday with a legislative package to handle the coronavirus pandemic, though Republicans don’t fully support it. The deal taking shape includes paid sick leave, nutrition aid and assistance for states, including unemployment and Medicaid costs.”
THESE MEASURES ARE VITALLY IMPORTANT. WHEN FACED WITH A DECISION TO STAY HOME WHEN SICK MEANS NO FOOD ON THE TABLE AND NO RENT CHECK, PEOPLE ARE MORE LIKELY TO MAKE THE DECISION TO FEED THEIR FAMILY and go to work. But that will expose others to the virus and cause a peak in infections, potentially overloading our medical system. The federal government must take measures that make it economically possible for sick folks to stay home and avoid rapidly infecting others.
Closing schools and shifting to on-line classes can help slow the spread.
FROM NPR: Every day for the past week, more than 100 colleges and universities around the country have canceled in-person classes and have taken the unprecedented step of moving classes online.
This is an important example of social distancing.
From NPR: “According to a report in Education Week, at least 10,600 schools have been closed or are scheduled to close for several weeks. That is a small but quickly growing fraction of the approximately 50 million K-12 students in the United States.”
But closing K-12 places some children at increased risk as discussed below.
PROTECTING OUR CHILDREN:
FROM NPR: The Life Kit team looks at what you need to know about working from home and parenting young children.
And from that website link here are some important quotes.
“Luckily, public health officials in King County, Washington, offer this helpful guidance:
“Social distancing doesn’t mean you have to stay stuck in your house. … The current recommendation is to avoid large groups. That mostly means groups over 50 people but conservatively means anything more than 10 people. However, if you don’t fall into the high risk group, you can still certainly visit each other.”
Think of it as a good opportunity for one-on-one hangouts.
Make sure they understand that hand-washing isn’t optional. And that means showing them how to do it properly: using soap, warm water and time. Washing should take 20 seconds, which means you may need to help them find a song they can sing (in their heads, maybe twice) — like the ABCs or “Happy Birthday” songs. Be sure they wash whenever they come in from outside, before eating, after coughing or sneezing or blowing their nose and, of course, after using the bathroom.
Just For Kids: A Comic Exploring The New Coronavirus
For younger kids, it can’t hurt to remind them that nose-picking is a no-go, and that they should cough into their elbows. If you’re feeling ambitious, clip their fingernails frequently, as they provide a sneaky hiding spot for viruses. Hand lotion keeps skin comfy and unbroken, which also helps prevent the spread of infection.
Closing schools is a complicated decision. Many school leaders and public health officials seem to be waiting for an infection or potential infection in their immediate school community before closing. While the science suggests closing schools earlier is more effective at slowing the spread of disease, it’s important to understand why so many school leaders are so reluctant to close schools.
For one thing, parents should understand that for many kids in the United States, being sent home from school is also a public health risk. Many children may not have parents who can take off work, or work from home, if school is canceled. They may also live in unsafe neighborhoods. Millions of U.S. children rely on schools for free or reduced-price meals, too, and 1.5 million schoolchildren nationwide are housing-insecure. For many of these kids, having to miss several weeks of school could be incredibly destabilizing.
A few more ideas: Try laundering things like coats, backpacks and reusable shopping bags more frequently and take off shoes when you come inside. For cleaning the house, the Centers for Disease Control and Prevention says “diluted household bleach solutions, alcohol solutions with at least 70% alcohol, and most common EPA-registered household disinfectants should be effective.”
If you have not read my first 2 posts about COVID19 please do so.
Remember, many infected people have no or little symptoms but they can still transmit the disease. High risk individuals include the elderly and those with chronic disease, especially cardiovascular disease, pulmonary (COPD, asthma, emphysema, smokers) and diabetics. Anyone on immune suppressive drugs is at very high risk.
Do everything you can to support your immune system:
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob
I spoke to a friend who was the Public Health Officer for Sacramento County for many years. She still consults on infectious disease and public health.
There is an important distinction between DROPLET spread and AEROSOL spread.
TB and measles are examples of AEROSOL spread. If someone coughs or sneezes in a room the particles can remain suspended in the air for long periods of time. So if you walk into the room after someone coughs or sneezes you can get the disease. This transmission requires “negative pressure” rooms in a hospital for isolation.
Corona virus and flu were believed to be different. They were thought to be spread by droplets which do not remain suspended in the air. The infected person must sneeze or cough droplets in your face or you must get the droplets from a contaminated surface (example: door knob) and then touch your face. In hospitals this requires only closing the door of the hospital room, not a negative pressure room (the negative pressure does not allow the aerosol to leave the room and it filters the room air).
Since this original post more scientific data have become available that strongly suggest that aerosol spread can occur with SARS CO2, (COVID-19) in community circumstances. Likelihood of transmission increases depending on many variables:
Masks and social distancing decrease spread.
Some never develop symptoms. Asymptomatic individuals can carry and transmit the virus.
In individuals who develop symptoms, transmission can occur several days before symptoms appear.
Surfaces like doorknobs, keyboards, tables are not as important as previously thought. If someone is sick OR infected but not symptomatic with COVID19, the virus was thought previously to be transmitted by contact with a surface like a doorknob. cleaning these surfaces with Clorox or similar virus killing antiseptics was considered essential. Now we know that transmission by that route is much less important. AEOROSOL TRANSMISSION is the primary mode of transmission.
Nevertheless, frequent handwashing (at least 20 seconds) would be prudent.
Important: PUBLIC HEALTH RECOMMENDATIONS FOR INDIVIDUALS OVER AGE 65 AND THOSE WITH CHRONIC DISEASE INCLUDE VACCINATION FOR PNEUMOCCOUS. Contracting pneumococcal pneumonia before or after COVID19 would be very dangerous.
It is unlikely that there will be an effective COVID19 vaccine for a long time, if ever. Why? Because corona viruses MUTATE QUICKLY. There has never been an effective corona virus vaccine. But huge resources are now devoted to developing a vaccine and new technologies and approaches are being tried. (This was posted March 12, 2020, 9 months later a vaccine was available. However the “MUTATE QUICKLY” concern has proven true. As of 11/12/2022 we are still dealing with rapidly developing mutations with increasing immune evasion characteristics. But we have PAXLOVID, a combination anti-viral that is very effective in reducing morbidity, mortality, and risk of LONG COVID.
In the context of the COVID 19 pandemic I will close with the usual summary.
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob
On March 10, 2020 a panel discussion/conference of Infectious Disease and PANDEMIC experts convened at UCSF (University of California San Francisco). Here are the panelists.
Unless bracketed, these are direct quotes of the panelists. This was forwarded to me by a physician friend whose colleague prepared it. The “I” refers to that colleague.
University of California, San Francisco BioHub Panel on COVID-19
March 10, 2020
So that is the synopsis provided by my friend’s colleague.
Unfortunately, the Trump administration has been dangerously incompetent in addressing-mitigating the public health and economic impact. Trump STILL HAS NOT DECLARED THIS A NATIONAL EMERGENCY!
Whitehouse spokespeople have stated Trump does not want to declare this an emergency because it would contradict his earlier statements that COVID19 is not a serious problem (he tweeted and stated it is less serious than the flu). If declared a NATIONAL EMERGENCY it would free up large amounts of money and resources for public health, FEMA, and economic assistance, yet it has not been done. INSTEAD, TRUMP is waiting for his son-in-law (who has no scientific training) to research COVID19 and make recommendations for national policy!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
SERIOUSLY???????????
This post and all posts are for informational, educational purposes and should not be taken as medical advice. Consult your health care practitioner for medical advise.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob