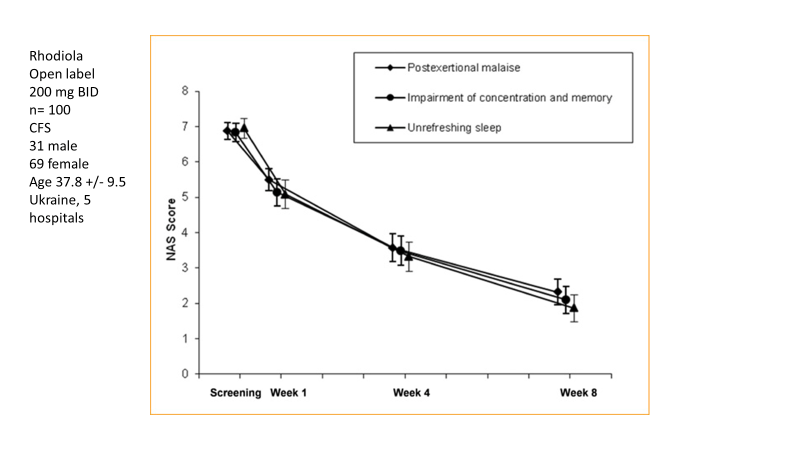
In his book Blindspots, Marty Makary MD (slated to be the next FDA commissioner) discusses why routine medical practices are often slow to change, despite mounting evidenced that those practices are not supported by best evidence. Although not discussed in his book, the evaluation and treatment of hypothyroidism presents a prime example of this problem. Before diving into the issues, lets review some basic physiology.
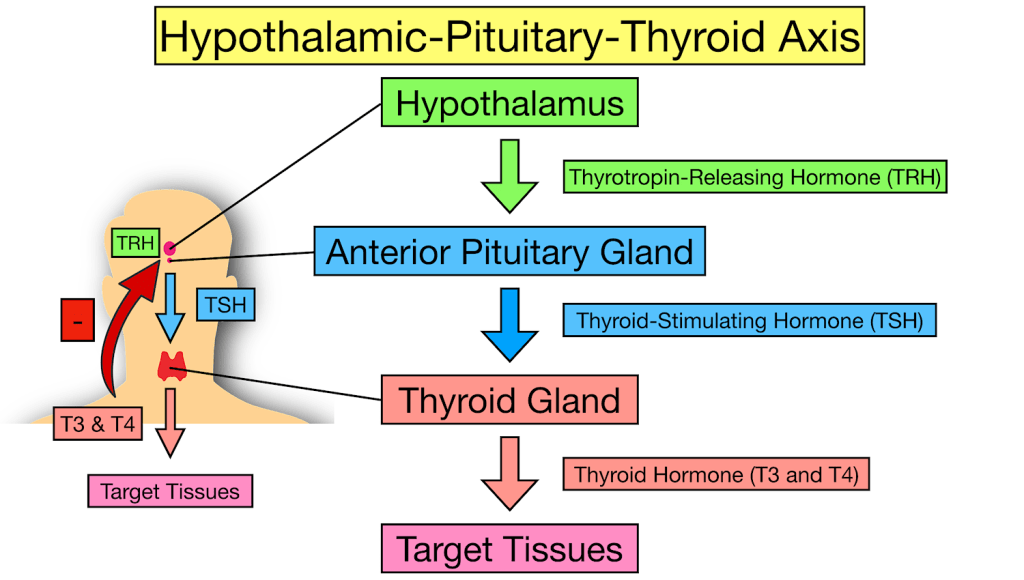
The hypothalamus in the brain produces TRH (thyrotropin releasing hormone) in response to circulating levels of T3 and T4 (two forms of thyroid hormone). TRH then stimulates production and release of TSH (thyroid stimulating hormone) in the pituitary gland. In turn, TSH stimulates the thyroid gland to produce thyroid hormone. The two forms of thyroid hormone produced by the thyroid gland are called T4 and T3 (T3 has 3 iodine molecules, T4 has 4) T4 is the predominant hormone produced by the thyroid gland. In the liver and the kidney T4 is converted to T3 through a process called deiodination, supplying 80% of circulating T3. Importantly, T3 is 7 to 10 times more potent than T4.
Both T3 and T4 directly inhibit TSH synthesis. This feedback system helps maintain homeostasis under conditions of optimal health. (https://www.ncbi.nlm.nih.gov/books/NBK278958/)

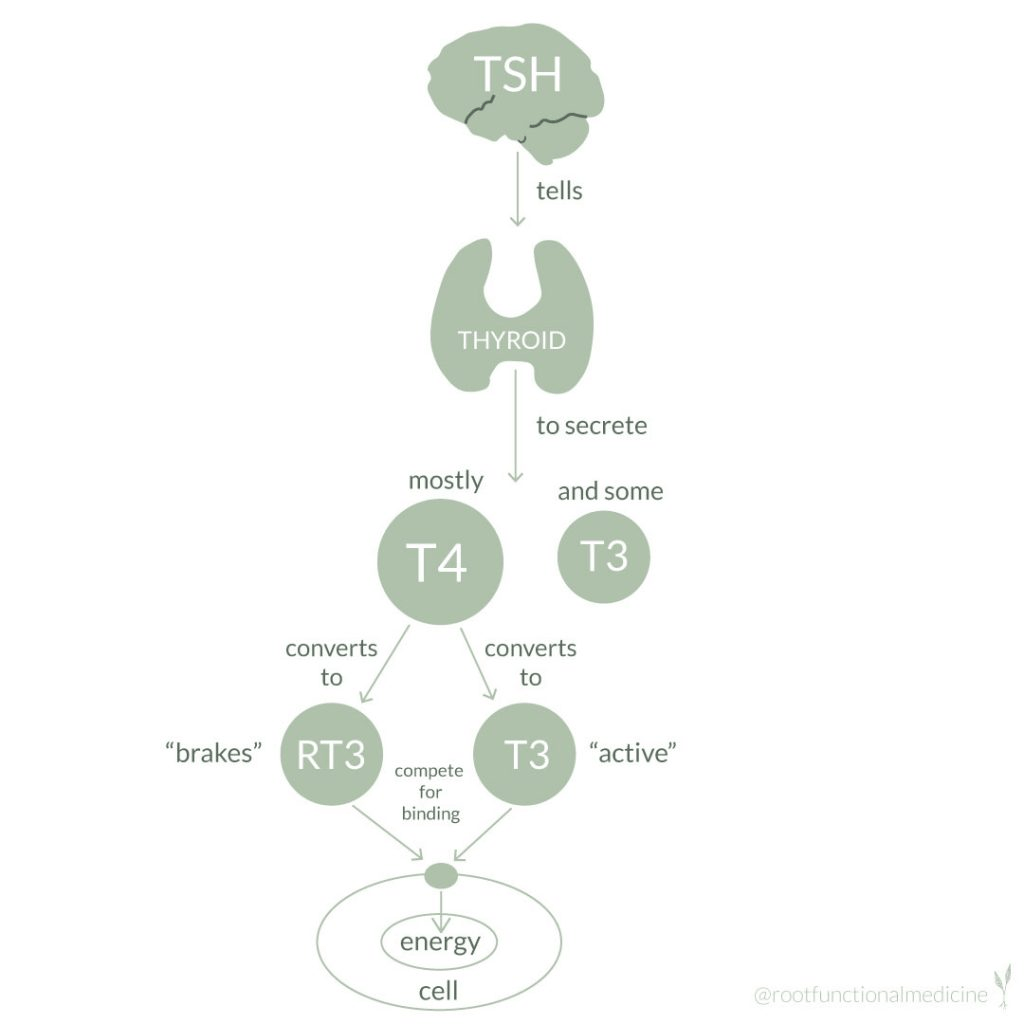
Taken from: https://rootfunctionalmedicine.com/conversion-of-t4-to-t3-thyroid-hormone/
When testing thyroid function, most physicians order only TSH (thyroid stimulating hormone) and T4. But to have normal thyroid function several conditions must be met. Of those many conditions, three are often not considered by most physicians and not evaluated with TSH and T4. First, there must be adequate conversion of T4 into T3, because T3 is the form of thyroid hormone that provides most physiologic effect. Second, there must be adequate transport of T4 and T3 into your cells. Third, levels of reverse T3 should not be high enough to block adequate amounts of Thyroid Hormone binding to receptors on your cells.
The “normal” range of TSH in most labs is 0.4 to 5.0 mU/L. Recently a narrower range of 0.5-2.5 mU/L has been proposed to exclude individuals with “minimal” thyroid dysfunction, but this is controversial. This controversy is the crux of one of the many problems in interpreting “normal” thyroid function tests. Proponents of the narrower range maintain that patients with symptoms of hypothyroidism and a TSH above 2.5 might benefit from treatment. In addition, proponents of the narrower range suggest that some patients with TSH levels above 2.5 may not report symptoms of hypothyroidism but their physiology may be suboptimal for health. (https://www.ncbi.nlm.nih.gov/books/NBK278958/) Physiology of the Hypothalamic-Pituitary-Thyroid Axis.
Treatment with T4 alone, may not provide adequate thyroid replacement.
If a physician orders only T4 and TSH to evaluate thyroid function, but conversion of T4 to T3 is impaired, a normal T4 and normal TSH will be interpreted as normal thyroid function. But with low T3 levels, a patient can experience symptoms of hypothyroidism. Likewise, if a patient is only treated with T4 (levothyroxine) but has issues converting T4 to T3, they may need to receive a prescription for T3 and T4. Using the ratio of Free T3 to Free T4 one can identify patients with problems caused by inadequate deiodination (conversion of T4 to T3). Monotherapy with levothyroxine (T4) has been standard of care for decades. But studies have demonstrated that patients treated with T4 only have relatively low serum levels of T3 (tri-iodothyronine) compared to the general population and symptoms of hypothyroidism persist for some patients despite normal TSH levels.
Issues of active versus passive transport.
T3 and T4 enter the hypothalamus and pituitary glands “passively”, meaning an active transport mechanism is not necessary. But in the rest of the body active transport of T3 and T4 into cells is necessary. If there is a problem with the active transport system, the hypothalamus and pituitary may “see” normal levels of T3 and T4 but the rest of the body may not be getting the full benefit of thyroid hormone. Thus, TSH levels will be normal, T4 levels will be normal, but cellular T3 and T4 levels will not be adequate. Yet physicians will interpret a normal TSH and T4 to mean normal thyroid function. Conditions that impair thyroid hormone transport into cells include: insulin resistance, diabetes, obesity, chronic and acute dieting, diabetes, depression, anxiety, bipolar disorder, neurodegenerative diseases, chronic fatigue syndrome, fibromyalgia, cardiovascular disease, inflammation and chronic illness, and disorders of lipid metabolism.
Reverse T3 can cause problems.
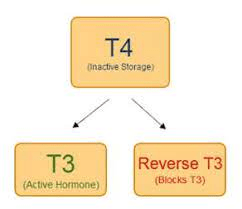
High levels of reverse T3 can occur under many conditions including chronic stress, chronic inflammation and many chronic diseases. As previously discussed, Reverse T3 binds to Thyroid hormone receptors but does not have the beneficial effect of normal T3, thus blocking T3 from doing its job. Most physicians do not measure reverse T3 or calculate the T3/reverse T3 ratio.
Therefore, in addition to problems with deiodinase (conversion of T4 to T3), high levels of reverse t3 can render monotherapy with levothyroxine inadequate, while leaving TSH and T4 levels “normal”.
How to calculate t3/reverse t3 ratio – National Academy of Hypothyroidism
This has been a quick discussion of a complex system. Not all aspects of thyroid testing and treatment have been addressed. Hopefully this discussion will help you understand why simply measuring TSH and T4 (a common practice) will not tell you whether you have normal thyroid function. Ideally, all patients being tested would have free T3 and reverse T3 measured in addition to T4 and TSH. In addition, the free T3/reverse T3 ratio and the free T3/freeT4 ratio would be considered when deciding whether treatment with T4 alone (levothyroxine monotherapy) is adequate. Many patients would benefit from adding T3 (triiodothyronine) to T4 (levothyroxine) therapy. In addition, a TSH level above 2.5 should be carefully evaluated for hypothyroid symptoms as levels above 2.5 are arguably “abnormal” (or at least should raise a red flag as to the possibility). Finally, recognize that this discussion presents controversies in medicine. Most practitioners apply the concept of “sick euthyroid” to patients with acute illness and low T3 levels, considering it a “normal” protective mechanism that does not require thyroid hormone therapy. But under chronic conditions, many practitioners who think “outside the box” would consider poor conversion of T4 to T3 and/or high levels of reverse T3, as possible indications for thyroid hormone therapy when symptoms of hypothyroidism are present. Under these circumstances directly addressing underlying causes such as chronic inflammation may provide the best initial approach. (anti-inflammatory diet, regular exercise, good sleep habits, stress reduction, strengthen social support)
But when a patient is already on monotherapy with T4, consideration of adding T3 to improve quality of life and physiologic function is worthy of consideration when comprehensive laboratory evaluation suggests problems as described above (cellular transport, T4 to T3 conversion, high reverse T3).
For a greater dive into this subject follow these links.
Physiology of the Hypothalamic-Pituitary-Thyroid Axis.
The relevance of T3 in the management of hypothyroidism – The Lancet Diabetes & Endocrinology
Levothyroxine Monotherapy Cannot Guarantee Euthyroidism in All Athyreotic Patients
Is a Normal TSH Synonymous With “Euthyroidism” in Levothyroxine Monotherapy?
Thyroid Hormone Transport into cellular tissue.
HPA axis dysfunction in Chronic Fatigue Syndrome and Fibromyalgia
Hormone replacement therapy in the geriatric patient, part 1.
Hormone replacement therapy in the geriatric patient, part 2.
Peripheral thyroid hormone conversion.
A complete pathway map of T4 and T3 metabolism and clearance
THIS WEBSITE PROVIDES INFORMATION FOR EDUCATIONAL PURPOSES ONLY. CONSULT YOUR HEALTH CARE PROVIDER FOR MEDICAL ADVICE.
Eat clean, drink filtered water, love, laugh, exercise outdoors in a greenspace, get some morning sunlight, block the blue light before bed, engage in meaningful work, find a sense of purpose, spend time with those you love, AND sleep well tonight.
Doctor Bob